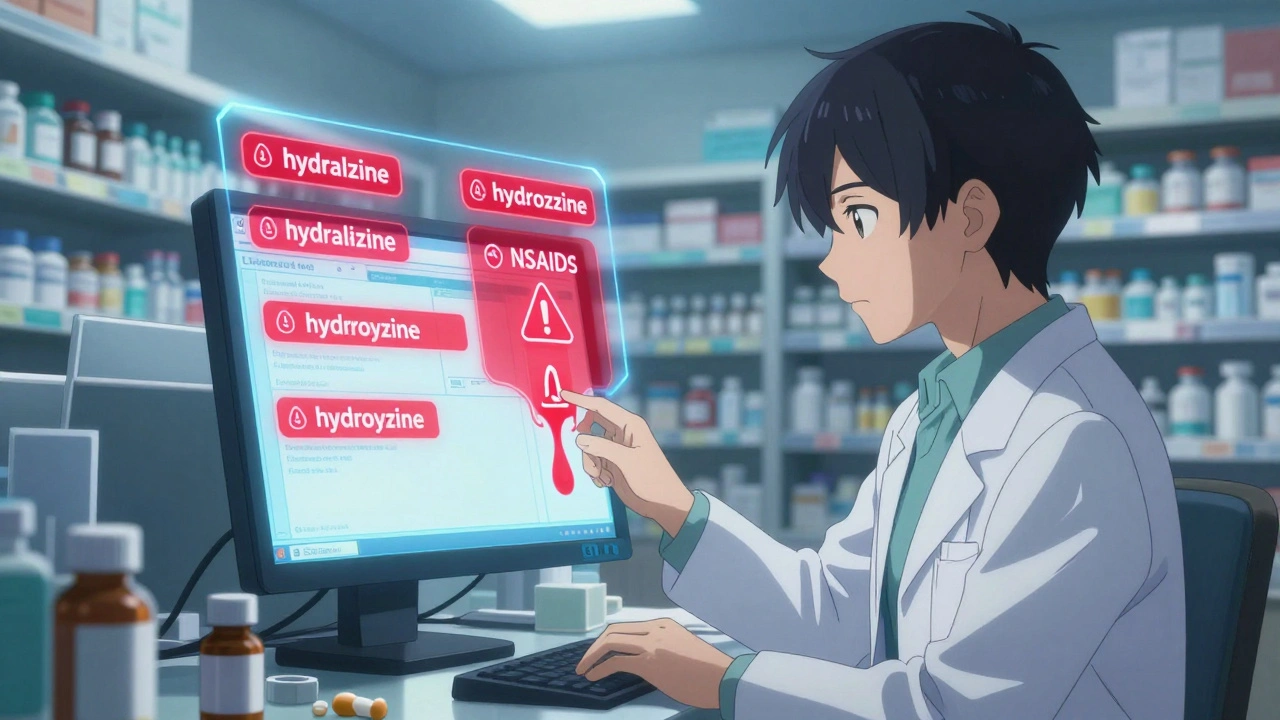
Every time you pick up a prescription, a pharmacist is doing something you rarely see but absolutely depend on: stopping a mistake before it hurts you. It’s not just about counting pills. It’s about catching a 10-fold overdose on warfarin, spotting a dangerous mix of blood thinners and NSAIDs, or realizing the wrong drug was prescribed because the names sound alike-like hydralazine and hydroxyzine. These aren’t hypotheticals. They happen daily. And pharmacists are the last line of defense.
The Final Check That Saves Lives
Pharmacists don’t just fill prescriptions. They review them. Every single one. In hospitals, community pharmacies, and long-term care facilities, pharmacists use their training to catch errors that slip through from doctors, nurses, or even automated systems. The Institute for Safe Medication Practices calls pharmacists the “last line of defense.” And they’re right. Studies show pharmacists intercept about 1 in 4 potentially harmful errors before a patient ever takes the medication. In the U.S. alone, medication errors affect 1.5 million people each year. But here’s the flip side: pharmacists prevent around 215,000 of those errors annually. That’s not luck. It’s a structured, skill-based process built on years of pharmaceutical science training. A pharmacist doesn’t just know what a drug does-they know how it interacts with every other drug, supplement, and condition a patient has. They see the full picture.How Errors Actually Happen
Most people assume errors come from doctors writing bad handwriting. That’s outdated. Today, 95% of prescriptions are electronic. So what’s left? - Wrong dose: A 75-year-old gets a kidney-damaging dose of ibuprofen because the system didn’t adjust for age or renal function. - Wrong drug: A patient with diabetes gets metformin instead of metoprolol because the names look similar on screen. - Drug interactions: A patient on blood thinners is prescribed a new antibiotic that boosts the anticoagulant effect, risking internal bleeding. - Missing allergies: A patient’s allergy to sulfa drugs isn’t flagged because it’s buried in an old record. - Duplicate therapy: Two different doctors prescribe the same drug, and neither knows the other did. These aren’t rare. A 2022 study in Tehran’s infectious disease ward found 112 medication errors among 861 patients. Doctors caused nearly half. Nurses caused the other half. Patients? Just 2.7%. The real problem? Systems that don’t talk to each other.Tools Pharmacists Use to Catch Errors
Modern pharmacies aren’t just shelves and counters. They’re high-tech safety hubs.- Electronic Health Records (EHRs) give pharmacists instant access to a patient’s full medical history-diagnoses, allergies, lab results, even past prescriptions.
- Clinical Decision Support Systems flag potential interactions, overdoses, or allergies in real time. These systems catch 85-90% of possible drug interactions-but they’re not perfect. Pharmacists still have to decide which alerts matter.
- Barcode Scanning is now standard in hospitals. Before a drug is given to a patient, the pharmacist or nurse scans the medication and the patient’s wristband. If they don’t match? The system stops everything. This cuts dispensing errors by 51%.
- Automated Dispensing Cabinets in hospitals only release medications when the right person, right drug, and right patient are confirmed. They reduce errors by 38%.
- Medication Reconciliation happens when a patient moves between care settings-like from hospital to home. Pharmacists compare every drug the patient was on before admission with what’s being prescribed now. On average, they find 2.3 errors per patient during this process.
The Double-Check System That Works
In community pharmacies, the most effective safety net isn’t technology-it’s people. The “double-check” system means a pharmacy technician reviews the prescription first, then the pharmacist reviews it again. This simple step prevents 78% of potential dispensing errors. Why? Because humans see things differently. A technician might notice the wrong bottle was pulled. The pharmacist might catch a dosage mismatch the technician missed. Together, they cover each other’s blind spots. In high-risk cases-like insulin, blood thinners, or chemotherapy-the law requires an independent double check. No exceptions. That’s because one mistake here can kill. Studies show this step cuts errors by 42% for these drugs.Where the System Fails
It’s not all perfect. Pharmacists are human. And systems can overwhelm them. One major problem? alert fatigue. Clinical systems throw up so many warnings-about drug interactions, allergies, dosing-that pharmacists start ignoring them. One study found pharmacists override 49% of alerts because they think they’re irrelevant. That’s dangerous. The fix? Tiered alerts. Newer systems now rank warnings by severity. A life-threatening interaction gets a red flag. A minor interaction gets a quiet pop-up. That reduces overrides to 28%. Another issue? Workload. In busy community pharmacies, pharmacists might be juggling 150 prescriptions a day. When you’re rushing, you miss things. One pharmacy technician in New Zealand told me she sees 3-4 serious errors every week that slip past pharmacists because they’re swamped. And in low-income countries or underfunded clinics, the problem is worse. One 2022 study found that when pharmacists are responsible for 500+ patients each, error reduction drops to just 15%. There’s no magic tool that fixes understaffing.Pharmacists Don’t Just Catch Errors-They Improve Care
The best pharmacists don’t stop at saying “no.” They say, “Here’s what we can do instead.” A patient on five medications for high blood pressure, diabetes, and arthritis? A pharmacist might realize two of those drugs do the same thing. They can suggest dropping one. That cuts side effects, saves money, and makes it easier for the patient to take their meds. Studies show pharmacist-led reviews improve therapeutic appropriateness by 28%. That means patients get better outcomes-not just safer ones. One patient on Yelp shared how a pharmacist caught a 10-fold overdose on warfarin. That’s the kind of story that doesn’t make headlines-but saves lives.Why Teamwork Matters More Than Ever
The most effective safety systems aren’t run by pharmacists alone. They’re run by teams. When pharmacists work with doctors, nurses, and technicians in coordinated care models, medication errors drop by 52%. That’s nearly double the reduction seen when pharmacists work alone. Why? Because errors start before the prescription hits the pharmacy. A doctor prescribes the wrong drug. A nurse transcribes it wrong. A system sends it to the wrong pharmacy. The pharmacist catches it-but the system should’ve stopped it earlier. Dr. David Bates from Harvard puts it bluntly: “Over-reliance on pharmacists creates system vulnerability.” The goal isn’t to make pharmacists do all the heavy lifting. It’s to build a system where errors are caught at every step.The Future: More Responsibility, Better Tools
Pharmacists are taking on more. In 27 U.S. states, they can now adjust medications under collaborative agreements-without waiting for a doctor’s approval. That’s huge for chronic disease management. New AI tools are helping too. Systems now use machine learning to flag the most dangerous prescriptions first, reducing pharmacists’ cognitive load by 35%. They’re not replacing pharmacists-they’re helping them focus on what matters. By 2026, the number of dedicated medication safety pharmacists is expected to grow by 22%. Hospitals are investing more. Regulators are requiring it. The Joint Commission now mandates medication reconciliation in every care transition. That’s a $1.2 billion opportunity for pharmacist services. But the biggest challenge? Workforce shortages. By 2025, the U.S. could be short 15,000 pharmacists. If we don’t fix that, even the best systems won’t help.What You Can Do
You don’t have to wait for a pharmacist to catch a mistake. You can help too.- Keep an updated list of all your medications-including vitamins and supplements-and bring it to every appointment.
- Ask your pharmacist: “Is this the right drug for me? Could it interact with anything else I take?”
- If a dose seems too high or too low, say something. You know your body better than any algorithm.
- Use one pharmacy for all your prescriptions. That way, your pharmacist sees your full picture.
How often do pharmacists catch medication errors?
Pharmacists prevent an estimated 215,000 medication errors each year in the U.S. alone. Studies show they intercept about 1 in 4 potentially harmful errors before a patient receives the medication. In hospital settings, they catch an average of 2.3 medication discrepancies per patient during transitions of care, like hospital discharge.
Can technology replace pharmacists in catching errors?
No. While electronic systems like CPOE and clinical decision support catch some errors, they miss others. Computer systems alone reduce errors by 17-25%. When pharmacists add their clinical judgment, error detection jumps to 45-65%. Algorithms can flag a possible interaction, but only a pharmacist can decide if it’s truly dangerous for that specific patient.
What’s the most common type of prescription error pharmacists catch?
The most common errors are wrong doses, drug interactions, and prescribing the wrong drug due to similar names (like hydroxyzine vs. hydralazine). Pharmacists also frequently catch duplicate therapies-when two doctors prescribe the same drug without knowing it. Allergies that aren’t properly recorded are another frequent issue.
Do pharmacy technicians help prevent errors too?
Yes. Pharmacy technicians are the first line of defense. They check National Drug Codes, verify prescriptions against patient records, and flag confusing drug names or packaging errors before the pharmacist reviews them. In double-check systems, technicians catch 78% of potential dispensing errors before they reach the pharmacist.
Why do some errors still get through despite all the checks?
Overworked pharmacists, alert fatigue from too many system warnings, and poor communication between prescribers and pharmacies are the top reasons. In high-volume settings, pharmacists may review 150+ prescriptions a day. When rushed, even experts miss things. Systems also don’t always update in real time-like if a patient’s allergy is recorded in one hospital but not another.
How can patients help prevent medication errors?
Patients can keep a current list of all their medications-including over-the-counter drugs and supplements-and share it with every provider. Ask your pharmacist: “Is this the right drug for me?” and “Could this interact with anything else I take?” Use one pharmacy for all prescriptions so your pharmacist has your full history. If a dose seems off, speak up.