Medication Driving Safety Calculator
Medication Driving Safety Calculator
Enter details about the medication you've taken to determine when it's safe to drive. Some medications can impair your ability to drive even if you don't feel it.
Enter your medication details to see when it's safe to drive.
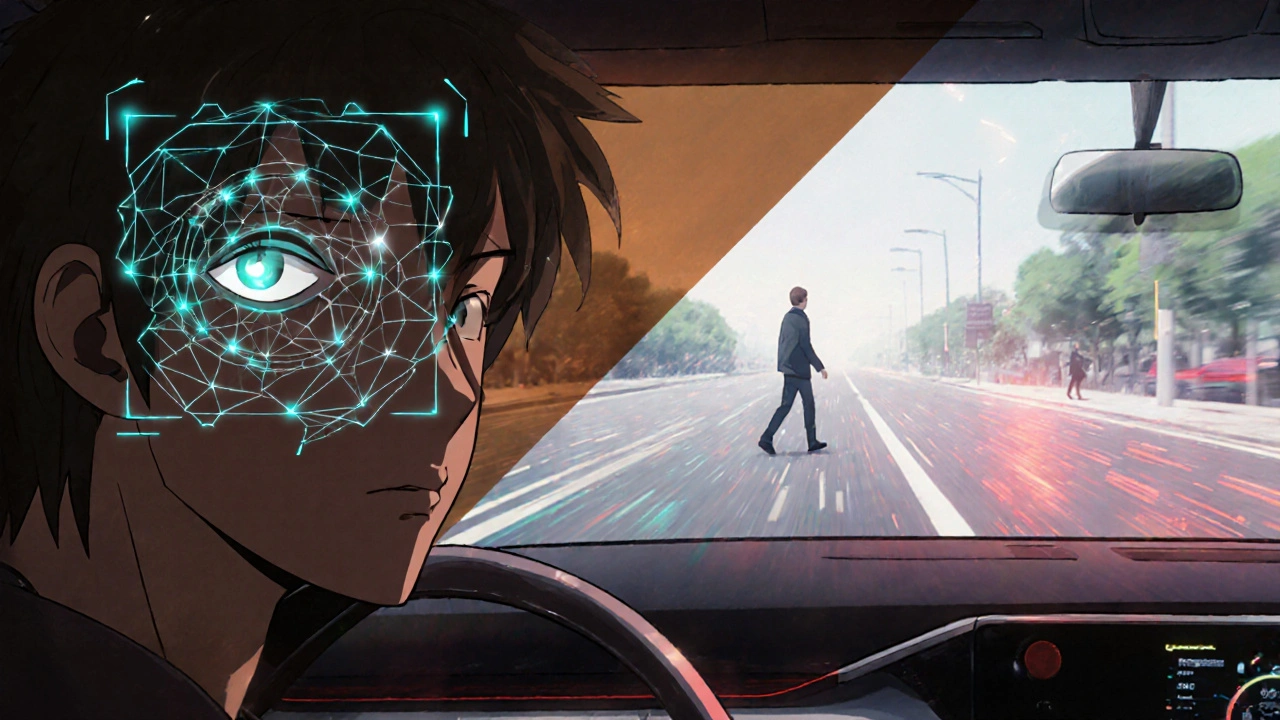
Driving on Medication Isn’t Always Safe - Even If You Feel Fine
Most people don’t think twice about taking a pill before getting behind the wheel. A sleep aid after a bad night. A painkiller for a sore back. An antihistamine for allergies. But what if that pill is slowing your reactions, blurring your vision, or making you drowsy without you even realizing it? Medications and driving is a dangerous mix that kills more people every year than most realize - second only to alcohol.
The truth is, you don’t have to be drunk to be impaired. A single dose of diphenhydramine - the active ingredient in Benadryl or Tylenol PM - can make you as unsafe behind the wheel as someone with a 0.10% blood alcohol level. That’s above the legal limit in every U.S. state. And you might not feel it. You might even feel wide awake. That’s the trick. These drugs don’t always announce their effects. They creep in quietly, and by the time you notice, it’s too late.
Which Medications Are Most Dangerous Behind the Wheel?
Not all medications affect driving the same way. Some are obvious. Others? Not so much. Here’s what the data shows:
- Benzodiazepines (like Xanax, Valium): These are prescribed for anxiety and insomnia, but they slow brain processing by 25-40%. Studies show they increase crash risk by 40-60%. Combine them with alcohol, and the effect multiplies.
- Opioids (like oxycodone, fentanyl): These cause drowsiness, slow reaction times by up to 300 milliseconds, and make your eyelids droop. Even at prescribed doses, they raise crash risk by 25-30%.
- First-generation antihistamines (like diphenhydramine, chlorpheniramine): Found in cold and allergy meds, these are silent killers. They cause drowsiness, poor coordination, and delayed decision-making - just like alcohol. NHTSA says they impair driving as much as a 0.10% BAC.
- Antidepressants (especially tricyclics and mirtazapine): These don’t just lift your mood. They can slow reflexes and reduce alertness. Research shows a 40% higher risk of motor vehicle crashes among users.
- NSAIDs (like ibuprofen, naproxen): You might think these are harmless. But studies show users have a 58% higher chance of being in a crash. The reason? Subtle changes in attention and reaction time that aren’t obvious until it’s too late.
- Sleep aids (like zolpidem/Ambien): These linger. Even if you slept 8 hours, the drug can still be active in your system 11 hours later. Many drivers take them at night and drive the next morning, thinking they’re fine - they’re not.
And here’s the kicker: second-generation antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) are much safer. They don’t cross the blood-brain barrier as easily. So if you need an allergy med, choose these - not the old-school ones.
Why You Think You’re Fine (But You’re Not)
One of the biggest dangers is self-misjudgment. People believe they can tell when they’re impaired. But the brain doesn’t work that way. If a drug is dulling your senses, it’s also dulling your ability to recognize that you’re dulling your senses.
Take the case of a Reddit user who took Tylenol PM at bedtime. They woke up at 7 a.m., felt fine, and drove to work at 9 a.m. - then failed a field sobriety test. The diphenhydramine was still in their system. They didn’t feel sleepy. But their brain was still sluggish. Their reaction time? Slowed. Their coordination? Off. Their judgment? Compromised.
A 2021 AAA survey found that 70% of drivers who took three or more potentially impairing medications still drove within two hours of taking them. Why? Because they didn’t know the risks. Only 32% of medication labels give clear timing guidance. Most just say “may cause drowsiness.” That’s not enough.

Legal Consequences Are Real - And Harsh
In the U.S., it’s illegal to drive while impaired by any drug - prescription, over-the-counter, or illegal. You don’t need to be caught with marijuana or cocaine. A single pill can get you arrested.
Every state has laws against drug-impaired driving. But unlike alcohol, there’s no universal legal limit for prescription drugs. Only 28 states have set specific blood concentration thresholds for medications. That means in the other 22, you can be convicted based on officer observation alone - even if your drug level is “within therapeutic range.”
And the penalties? They’re the same as DUI: license suspension, fines, mandatory classes, jail time, and a permanent criminal record. Insurance rates spike. Employers may fire you. And if you hurt someone? You could face felony charges.
There’s no “I didn’t know” defense. Courts don’t care if your doctor didn’t warn you. If you drove while impaired, you’re responsible.
Who’s at Highest Risk?
Older adults are the most vulnerable. After age 65, the body changes. It processes drugs slower. The liver and kidneys don’t clear medications as efficiently. Sensitivity to sedatives increases. And many seniors take multiple prescriptions - often without realizing how they interact.
According to the Beers Criteria (updated in 2019), 30+ medications should be avoided in adults over 65 because of their driving risks. Yet only 41% of physicians routinely discuss driving safety when prescribing them. Pharmacists are better - 89% now warn patients - but that still leaves millions at risk.
And it’s not just seniors. Young adults on ADHD stimulants, chronic pain patients on opioids, and people on antidepressants are all at elevated risk. The problem is widespread. In 2022, NHTSA found prescription drugs in 17.8% of impaired drivers - more than illicit drugs.
What You Can Do - Practical Steps to Stay Safe
You don’t have to give up your meds. But you do need to manage them wisely.
- Ask your doctor and pharmacist: “Could this affect my driving?” Don’t assume they’ll bring it up. Be specific. Ask about timing, duration, and interactions.
- Read the label - really read it. Look for words like “drowsiness,” “dizziness,” “blurred vision,” or “do not operate machinery.” That includes your car.
- Wait before you drive. For first-gen antihistamines, wait 4-6 hours. For sleep aids like Ambien, wait 8-12 hours. If you’re unsure, don’t drive.
- Test yourself. After taking a new med, try a short drive in a safe area - maybe around your neighborhood. Pay attention: Are you slower to react? Do you feel foggy? Do you miss exits? If yes, don’t drive.
- Avoid combinations. Mixing meds with alcohol, marijuana, or even caffeine can amplify impairment. A 2020 study found 22% of trauma patients had multiple drugs in their system - and the effects were worse than expected.
- Choose safer alternatives. Need an allergy med? Pick Claritin or Zyrtec over Benadryl. Need pain relief? Talk to your doctor about non-sedating options.
There’s even a free tool called the Driving Simulator Test from the University of Iowa. It takes 15 minutes and checks your reaction time, lane control, and decision-making. If you’re on multiple meds, try it. It’s not perfect - but it’s better than guessing.
The Future: Tech Is Trying to Help
Change is coming - slowly. In May 2023, the FDA started requiring “Driving Risk Scores” on medication labels, rating impairment from 1 (minimal) to 5 (severe). That’s a big step.
NHTSA’s new saliva tests can now detect 12 common prescription drugs on the roadside with 92.7% accuracy. And by 2027, most new cars will have sensors that monitor eye movement and steering patterns to detect drowsiness or impairment.
But technology won’t fix everything. The real fix is awareness. People need to know that a pill isn’t just a pill. It’s a tool - and like any tool, it can be dangerous if used carelessly.
Final Thought: Your Life Is Worth More Than Convenience
It’s easy to say, “I’ll just take one and drive.” But one pill can change everything. One moment of carelessness can end a life - yours, or someone else’s.
Medications help. But they don’t make you invincible. Driving requires sharp focus, quick reflexes, and clear judgment. If your meds are stealing those, you’re not just risking a ticket. You’re risking your freedom, your future, and the lives of others.
Don’t wait for an accident to learn the lesson. Ask the questions. Read the labels. Wait it out. Choose safer options. Your next drive could be your last - if you don’t take it seriously.
Can I drive after taking ibuprofen or naproxen?
While NSAIDs like ibuprofen and naproxen don’t cause obvious drowsiness, research shows they increase crash risk by 58%. They can subtly reduce attention and slow reaction time, especially with long-term use. If you’re new to these meds, avoid driving for the first few hours until you know how they affect you.
Is it safe to drive after taking Benadryl?
No. Benadryl contains diphenhydramine, which impairs driving as much as a 0.10% blood alcohol level - higher than the legal limit in all U.S. states. Even if you feel awake, your reaction time and coordination are compromised. Wait at least 4-6 hours after taking it before driving.
Can my doctor be held responsible if I crash after taking a prescribed drug?
Legally, no. The law holds the driver responsible, not the doctor. But if your doctor failed to warn you about known risks - especially for high-risk medications - you may have grounds for a medical negligence claim. Still, the burden of safe driving always falls on you.
What should I do if I’m on multiple medications?
Ask your pharmacist for a medication review. Many offer free consultations. List every pill, including supplements and OTC drugs. Ask which ones could interact or impair driving. Use the Beers Criteria as a reference for older adults. Never assume combinations are safe - synergy can make impairment worse than expected.
Are there any medications that are safe to drive after taking?
Yes. Second-generation antihistamines like loratadine (Claritin), cetirizine (Zyrtec), and fexofenadine (Allegra) are much less likely to impair driving. Most non-sedating pain relievers (acetaminophen) and thyroid medications are also safe. But always check the label and monitor your own response.
Can I be tested for prescription drugs during a traffic stop?
Yes. Police can use saliva tests, blood tests, or a Drug Recognition Expert (DRE) evaluation to detect prescription drugs. Unlike alcohol, there’s no breathalyzer for pills - but officers are trained to spot signs of impairment. Refusing a test can lead to automatic license suspension under implied consent laws.
What should I do if I feel impaired after taking my medication?
Don’t drive. Call a friend, use a ride-share, or wait. If you’re unsure, err on the side of caution. Keep a backup plan ready - like a list of local ride services or a trusted person you can call. Your safety and others’ are worth more than saving time.

