More than half of adults over 65 struggle with sleep. They lie awake at night, wake up too early, or feel exhausted all day. It’s common. But what’s not common-and not safe-is reaching for a pill to fix it. Many seniors are prescribed sleep meds that were never meant for their bodies. These drugs can cause falls, memory loss, confusion, and even raise the risk of dementia. The truth? There are far safer ways to sleep well as you age.
Why Most Sleep Pills Are Risky for Seniors
Drugs like zolpidem (Ambien), triazolam (Halcion), and benzodiazepines such as lorazepam were designed for younger adults. Their chemistry doesn’t play well with aging bodies. As we get older, our liver and kidneys slow down. That means drugs stick around longer. A pill that wears off in 4 hours for a 30-year-old might last 12 hours in a 75-year-old. That’s why so many seniors wake up groggy, wobbly, and at risk of falling.
The American Geriatrics Society has been warning doctors since 1991. Their Beers Criteria-a trusted guide for safe prescribing in older adults-lists 10 sleep medications as potentially dangerous for seniors. Benzodiazepines? Avoid. Z-drugs like Ambien? Use only as a last resort. Even trazodone, often prescribed off-label for sleep, can cause dizziness and low blood pressure.
One study in the BMJ found that long-term use of benzodiazepines increased Alzheimer’s risk by 51%. Another showed seniors on these drugs were 30% more likely to fall. And falls? They’re not just bruises. They’re broken hips, long hospital stays, loss of independence. The risk isn’t theoretical. It’s happening in living rooms, hallways, and nursing homes across the country.
What the Experts Say: CBT-I Is the Gold Standard
There’s a better way. It doesn’t involve pills. It’s called cognitive behavioral therapy for insomnia, or CBT-I. It’s not a quick fix. It’s a process. But it works better than any medication-and lasts longer.
CBT-I teaches you how to retrain your brain and body for sleep. It’s not about counting sheep. It’s about fixing habits. If you’ve been lying in bed for hours awake, your brain starts associating your bed with stress, not sleep. CBT-I helps break that cycle.
Here’s what it typically involves:
- Sleep restriction: You limit time in bed to match how much you actually sleep. No more 8-hour bed time if you’re only sleeping 5 hours. This builds sleep pressure.
- Stimulus control: Bed is for sleep and sex only. No TV, no phone, no reading. If you’re not asleep in 20 minutes, get up and go to another room until you feel sleepy.
- Cognitive restructuring: You challenge thoughts like “I’ll never sleep” or “If I don’t sleep tonight, I’ll be useless tomorrow.” These thoughts keep you awake.
- Sleep hygiene: Not just “avoid caffeine.” It’s about consistent wake times, daylight exposure, and avoiding long naps.
Studies show CBT-I works. In one 2019 JAMA Internal Medicine trial, 57% of seniors over 60 who did telehealth CBT-I no longer met the criteria for insomnia after 8 weeks. And 89% stuck with it. Compare that to sleep meds, where most people stop taking them within a year because of side effects.
The Newer, Safer Sleep Meds (If You Really Need One)
Some seniors do need medication-sometimes temporarily. If a doctor says yes, there are safer options. These aren’t perfect, but they’re better than the old standards.
Low-dose doxepin (Silenor) is a tiny dose of an old antidepressant-3 to 6 mg. It doesn’t cause next-day grogginess or confusion. It works by blocking histamine, not by sedating your brain like benzodiazepines. In studies, it improved sleep time by nearly 30 minutes with side effects barely higher than placebo.
Ramelteon (Rozerem) mimics melatonin. It helps you fall asleep faster by targeting your body’s natural sleep clock. It’s not addictive. It doesn’t cause memory problems. Dose: 8 mg, taken 30 minutes before bed. Side effects? Very rare.
Lemborexant (Dayvigo) is the newest. It blocks orexin, the brain chemical that keeps you awake. It’s been tested in adults 55+. Compared to zolpidem, it caused less dizziness and postural instability. Half-life? About 17 hours-long enough to help you stay asleep, short enough to avoid morning fog.
But here’s the catch: cost. Low-dose doxepin and ramelteon can cost $400 a month without insurance. Generic zolpidem? $15. That’s why many seniors stay on the risky stuff-even when their doctor knows it’s not ideal.

What to Avoid: The Dangerous Ones
Some sleep drugs should never be used in seniors. Period.
- Triazolam (Halcion): A short-acting benzodiazepine. It’s especially risky because it can cause memory blackouts and confusion. The Beers Criteria says: avoid.
- Flurazepam (Dalmane): A long-acting benzodiazepine. It lingers in the body for days. Increases fall risk by 50%.
- Zolpidem (Ambien) over 5 mg: The FDA warns that 10 mg doses can cause next-day impairment. For seniors, 5 mg is the max. Even then, use sparingly.
- Over-the-counter sleep aids with diphenhydramine (Benadryl, ZzzQuil, Tylenol PM): These are anticholinergics. They dry out your mouth, blur your vision, and scramble your memory. Long-term use is linked to higher dementia risk.
These aren’t just “use with caution.” They’re red flags. If your doctor prescribes one of these, ask why. Ask for alternatives.
Deprescribing: How to Safely Stop Sleeping Pills
If you’ve been on a sleep med for months-or years-stopping suddenly can make insomnia worse. That’s called rebound insomnia. It’s why many people feel trapped.
The key is tapering. Slowly. Under supervision.
Here’s how it works:
- Work with your doctor. Don’t quit cold turkey.
- Reduce dose by 10-25% every 1-2 weeks. For example, if you take 10 mg of zolpidem, go to 7.5 mg for two weeks, then 5 mg.
- Use CBT-I tools during tapering. Sleep restriction and stimulus control help your body relearn natural sleep.
- Track your sleep. Use a notebook or app. Note how you feel in the morning. Are you less dizzy? Clearer-headed?
- Give it time. It can take 4 to 8 weeks to fully stop. Some people need longer.
The STOPP/START criteria-a tool used by pharmacists and geriatricians-recommends this exact approach. It’s not easy. But it’s worth it. One woman in her 70s told me she went from 2 mg of Lunesta every night to none at all. After 6 weeks of CBT-I, she sleeps better than she has in 20 years.
Non-Medication Strategies That Actually Work
You don’t need a prescription to improve sleep. Here’s what really helps:
- Get sunlight in the morning. Even 15 minutes helps reset your circadian rhythm. Sit by a window. Walk outside.
- Move during the day. Walking 30 minutes, 5 days a week, improves sleep quality more than most sleep meds.
- Keep a consistent wake time. No matter what time you went to bed, wake up at the same time every day-even weekends. This is the single most powerful sleep habit.
- Limit fluids after 7 PM. Fewer nighttime bathroom trips mean fewer awakenings.
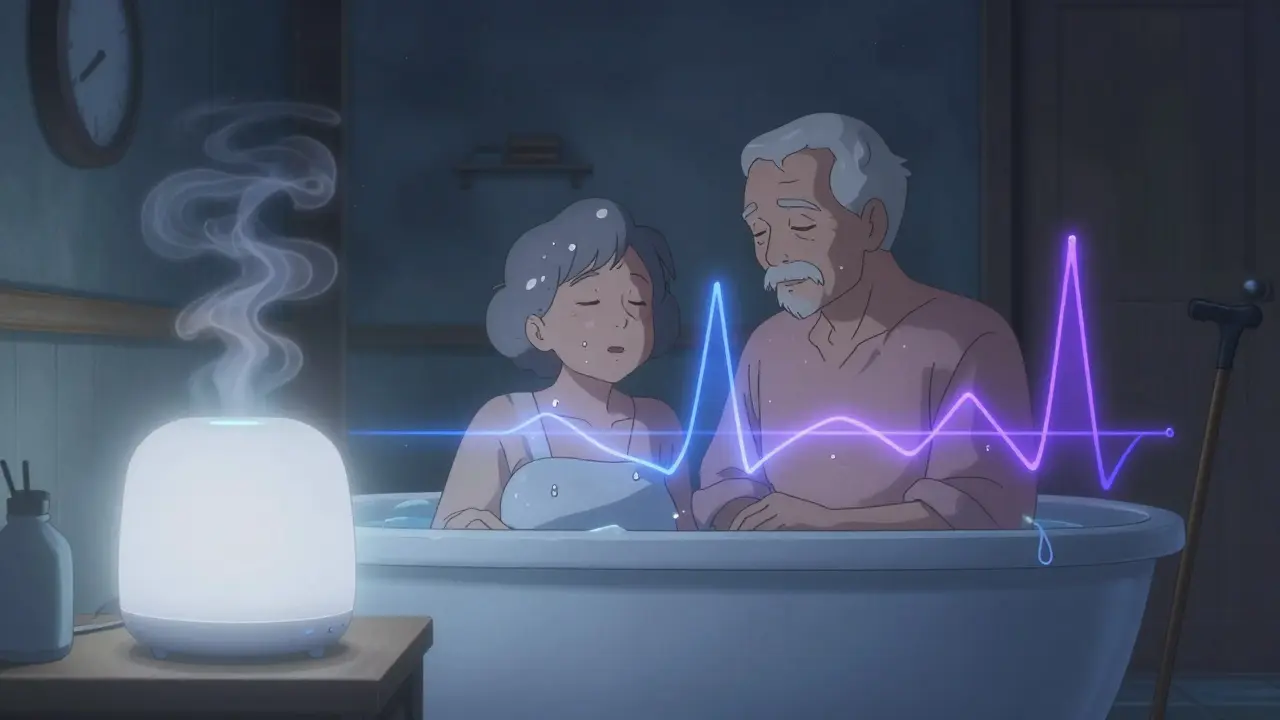
- Try a warm bath before bed. A 2023 study found that a 10-minute bath at 104°F, 1-2 hours before bed, helped seniors fall asleep 10 minutes faster.
- Use a white noise machine. Not for music. Just steady sound. It masks creaking floors, snoring, or traffic.
And don’t underestimate digital CBT-I. Apps like Sleepio and CBT-I Coach offer guided programs. One 2023 study in JAMA Neurology found 63% of seniors using Sleepio saw major improvements-same as in-person therapy.
When to Call Your Doctor
Not every sleep problem is insomnia. Sometimes, it’s sleep apnea. Or restless legs. Or depression. Or a medication side effect.
Call your doctor if:
- You snore loudly or stop breathing at night
- You feel tingling or crawling in your legs when trying to sleep
- You wake up confused or disoriented
- You’ve been on a sleep med for more than 3 months
- You’ve had a fall or near-fall
Bring your pill bottles. Ask: “Is this still right for me?” Don’t be afraid to push back. You’re not being difficult-you’re being smart.
Final Thought: Sleep Is a Right, Not a Reward
Good sleep isn’t a luxury. It’s essential. It protects your brain, your heart, your balance. You don’t have to settle for pills that make you drowsy, confused, or at risk of falling. The science is clear: CBT-I works. Safer meds exist. And you don’t have to take them forever.
Start small. Talk to your doctor. Try one non-medication strategy this week. Maybe it’s a morning walk. Or turning off screens an hour before bed. Maybe it’s asking for a referral to a sleep specialist.
Your body isn’t broken. It just needs the right conditions to rest. And you deserve that rest-without a pill.

