Colorectal cancer is one of the most preventable cancers-if caught early. Yet too many people wait until symptoms appear, by which time treatment becomes harder, costlier, and less effective. The good news? Screening works. Colonoscopy can find and remove precancerous polyps before they turn into cancer. And if cancer is found, modern chemotherapy regimens offer real hope, even for advanced cases. This isn’t just about medical jargon-it’s about knowing when to get screened, what to expect, and how treatment has changed in the last few years.
When Should You Start Screening?
For years, the standard was to start colorectal cancer screening at age 50. That changed in 2021. Now, major health organizations-including the U.S. Preventive Services Task Force, the American Cancer Society, and the American College of Gastroenterology-all recommend starting at age 45 for people at average risk. Why? Because rates of colorectal cancer in younger adults have been rising steadily. Between 1995 and 2019, incidence in people under 50 climbed by 2.2% each year. Rectal cancer, in particular, has surged. This isn’t a fluke. It’s a trend backed by millions of patient records and decades of research.That means if you’re 45 or older, you’re now in the target group. If you’re between 45 and 75, screening is strongly recommended. Between 76 and 85, the decision becomes more personal-based on your health, life expectancy, and whether you’ve been screened before. After 85, screening is generally not advised unless there’s a very specific reason.
But if you have a family history of colorectal cancer, a genetic syndrome like Lynch syndrome or familial adenomatous polyposis (FAP), or inflammatory bowel disease like ulcerative colitis, your doctor may recommend starting even earlier-sometimes in your 20s or 30s. These cases need a tailored plan, usually starting with colonoscopy and repeating more often.
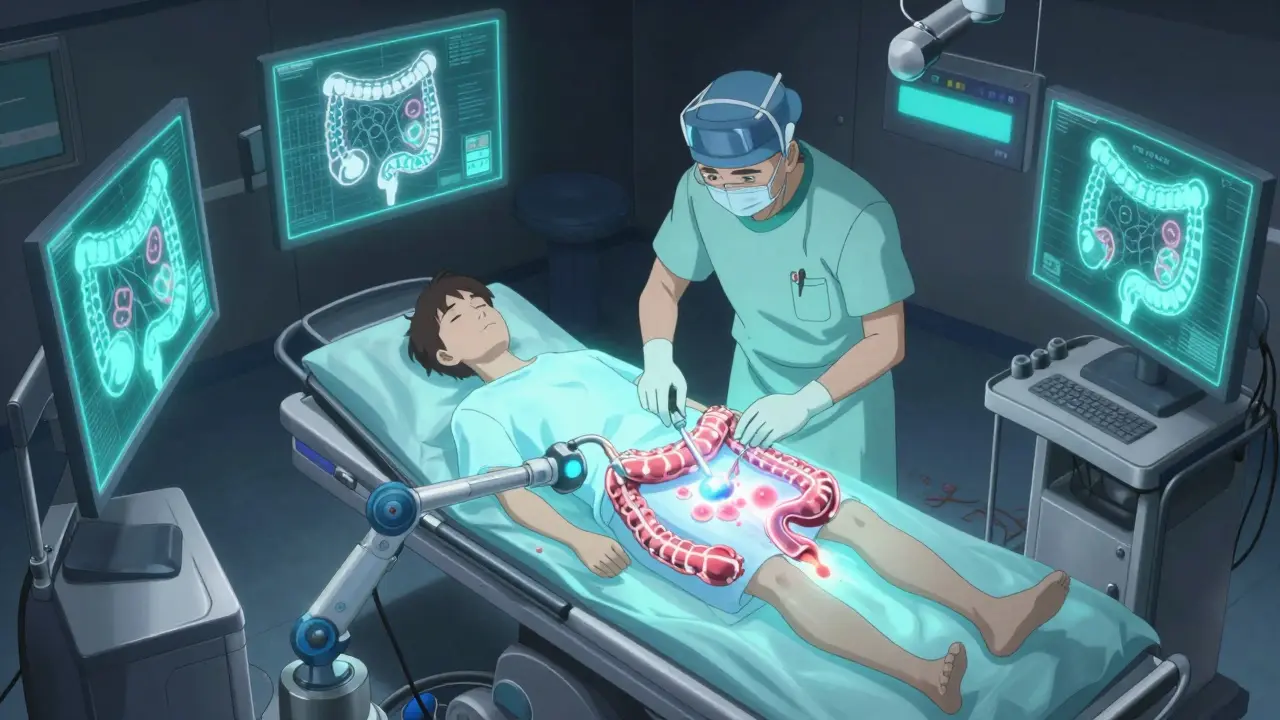
Colonoscopy: The Gold Standard
Colonoscopy is still the most effective screening tool. It’s the only test that can both find and remove polyps during the same procedure. That’s huge. Removing polyps can stop cancer before it starts. Studies show colonoscopy reduces colorectal cancer deaths by 65% and cuts cancer incidence by 67% over time.The procedure itself takes about 30 to 60 minutes. You’re sedated, so you won’t feel anything. But the prep? That’s what most people dread. You’ll need to drink a large volume of laxative solution-usually polyethylene glycol (PEG)-to clear your colon. It’s unpleasant. Many describe it as the worst part. But it’s necessary. A clean colon means the doctor can see everything. If the prep is incomplete, they might miss something.
After the procedure, you’ll need someone to drive you home. Side effects are rare but can include bloating, cramping, or minor bleeding if a polyp was removed. Serious complications like perforation happen in about 1 out of every 1,000 to 1,500 colonoscopies. That’s low, but it’s why choosing an experienced provider matters.
Once you’ve had a normal colonoscopy, you won’t need another for 10 years-if no polyps were found. If you had one or two small, low-risk polyps, you might need a repeat in 5 to 7 years. More polyps or larger ones mean you’ll need to come back sooner.
Other Screening Options
Not everyone wants a colonoscopy. That’s okay. There are other options, each with pros and cons.- Fecal Immunochemical Test (FIT): You collect a stool sample at home. It checks for hidden blood, which can signal cancer or large polyps. It’s simple, cheap, and non-invasive. But you have to do it every year. And if it’s positive, you still need a colonoscopy. Adherence is higher than colonoscopy in underserved communities-about 67% complete it compared to 42% for colonoscopy.
- Stool DNA Test (sDNA-FIT): This looks for both blood and DNA changes linked to cancer. It’s more sensitive than FIT, catching 92% of cancers versus 74%. But it’s also more expensive and has more false positives, meaning more people get called back for unnecessary colonoscopies.
- Flexible Sigmoidoscopy: Only examines the lower third of the colon. Less prep, no sedation. Reduces cancer risk in the lower colon by 26%. But it misses polyps higher up, so it’s not as complete as colonoscopy.
- CT Colonography (Virtual Colonoscopy): Uses X-rays to create a 3D image of your colon. No sedation, but you still need bowel prep. It can’t remove polyps, so any abnormality requires a follow-up colonoscopy. Plus, you’re exposed to low-dose radiation.
Stool tests are great for people who avoid clinics, live in rural areas, or can’t take time off work. But they’re not a substitute for colonoscopy if you’re high-risk. And they don’t prevent cancer-they only detect it.
What Happens If Cancer Is Found?
If a colonoscopy finds cancer, the next step is staging. That means figuring out how far it’s spread. Stage I means the cancer is small and hasn’t left the colon wall. Stage IV means it’s spread to distant organs like the liver or lungs.Treatment depends on the stage. Early-stage cancers (Stage I and II) are often cured with surgery alone. The surgeon removes the section of colon with the tumor and nearby lymph nodes. No chemo needed.
For Stage III, where cancer has reached nearby lymph nodes, chemotherapy is standard. The goal isn’t just to kill remaining cancer cells-it’s to prevent recurrence. The most common regimen is CAPOX (capecitabine and oxaliplatin) or FOLFOX (5-fluorouracil, leucovorin, and oxaliplatin). Both are given over 6 months. Side effects include nerve damage (tingling in hands and feet), fatigue, nausea, and lowered blood counts. Oxaliplatin can cause cold sensitivity-some patients can’t even hold an ice cube.
For Stage IV, the goal shifts from cure to control. Chemotherapy extends life and improves quality of life. Regimens are similar but often include targeted drugs like bevacizumab (Avastin), cetuximab (Erbitux), or panitumumab (Vectibix). These drugs block specific proteins cancer cells use to grow. They’re not for everyone-your tumor’s genetic profile determines which ones might work. Testing for mutations in KRAS, NRAS, and BRAF genes is now routine before starting treatment.
Immunotherapy is becoming an option for a small group-patients with mismatch repair deficiency (dMMR) or microsatellite instability-high (MSI-H) tumors. Drugs like pembrolizumab (Keytruda) can trigger the immune system to attack cancer cells. In some cases, these patients see long-term remission without chemotherapy.

Why Screening Rates Are Still Too Low
Despite all the evidence, only 67% of adults aged 50 to 75 in the U.S. are up to date with screening. That’s below the national target of 70.5%. Why? Several reasons:- Access: In rural areas, wait times for colonoscopy can be over two months. There aren’t enough endoscopists.
- Cost: Uninsured people are far less likely to get screened-only 58% compared to 78% for those with private insurance.
- Education: Many people don’t understand the difference between screening and diagnosis. They think, “I feel fine, so I don’t need it.”
- Disparities: African Americans have higher rates of colorectal cancer and higher death rates-but are 20% less likely to be screened.
Successful programs fix these gaps. Patient navigators-who help people schedule appointments, get transportation, and understand insurance-boost screening completion by 35%. Automated reminders from clinics increase adherence by 28%. Team-based care, where nurses and medical assistants handle prep instructions and follow-ups, cuts no-show rates by 42%.
What’s Next?
The future of screening is getting smarter. Blood tests that detect cancer DNA are in late-stage trials. One called Guardant SHIELD showed 83% sensitivity for colorectal cancer in a 10,000-person study. AI tools are already in use-Medtronic’s GI Genius system helps doctors spot polyps during colonoscopy that might be missed. It boosts detection rates by 14%.Soon, screening may become personalized. Instead of everyone getting a colonoscopy at 45, your risk score-based on genetics, diet, weight, smoking, and family history-could determine whether you start at 40, 50, or even 55. This could cut unnecessary procedures by 30% while keeping outcomes strong.
But until then, the simplest, most proven thing you can do is get screened. If you’re 45 or older, talk to your doctor. Don’t wait for symptoms. By the time you feel pain, bloating, or blood in your stool, it might be too late. Colonoscopy isn’t fun. But it’s life-changing. And if cancer is found early, your chances of living a full, normal life are over 90%.

