Medication Dry Eye Risk Calculator
Your Dry Eye Risk Assessment
Enter the medications you're currently taking. This tool identifies which ones may cause dry eyes and assesses your risk level.
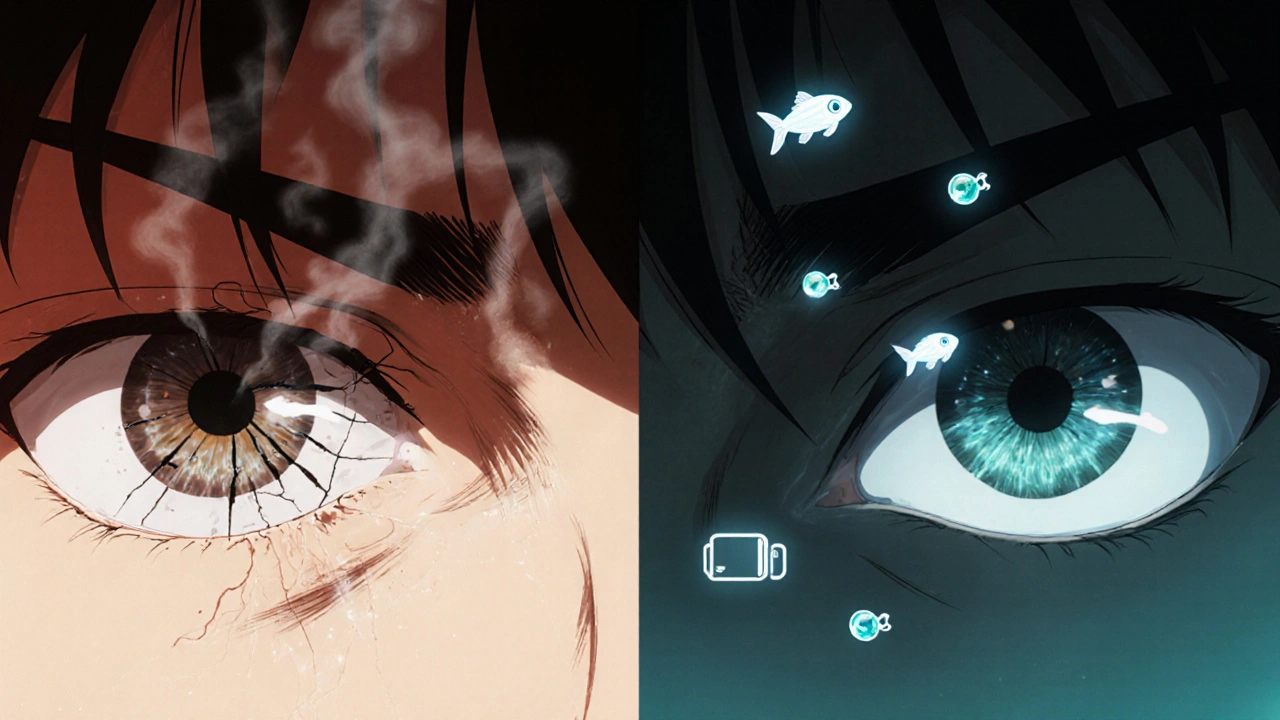
Many people don’t realize that the pills they take every day could be drying out their eyes. If you’ve been squinting at your screen, blinking more than usual, or feeling like there’s sand in your eyes-especially after starting a new medication-it’s not just fatigue. It’s likely medication-induced dry eye. This isn’t rare. About 1 in 4 people with dry eyes have it because of their meds. For those over 65, that number jumps to 4 in 10. You’re not imagining it. Your eyes are reacting to what’s in your bloodstream.
Which Medications Cause Dry Eyes?
It’s not just one drug. Dozens of common prescriptions and even over-the-counter pills can mess with your tear production. Antihistamines like Benadryl, Claritin, and Zyrtec are big offenders. They block signals your body uses to make tears. Antidepressants-especially SSRIs like Zoloft and Prozac, and older tricyclics like amitriptyline-do the same. Blood pressure meds like metoprolol and diuretics like Lasix pull fluid out of your system, including your eyes. Even acne treatment like Accutane can permanently damage the oil glands in your eyelids, which keep tears from evaporating too fast.Then there are the eye drops themselves. Glaucoma drops with benzalkonium chloride (BAK) preservative cause burning and dryness in nearly half of users. That’s right: the very treatment meant to protect your vision might be hurting your eyes. Switching to preservative-free versions cuts those symptoms by more than half.
How Lubrication Works-And What Actually Helps
Artificial tears sound simple, but not all are created equal. Preserved drops are fine for occasional use-once or twice a day. But if you’re using them four or five times daily, you’re adding chemicals that irritate your eyes over time. That’s why ophthalmologists recommend preservative-free tears for daily management. They come in single-use vials, and you toss them after one use. No preservatives. No buildup. Just clean moisture.For people on glaucoma meds, timing matters. Apply your preservative-free tears 15 minutes before and after your eye drops. Studies show this simple trick improves symptoms in 78% of cases. It gives your eyes a buffer so the medication doesn’t wash away the lubrication-or vice versa.
For stubborn cases, prescription drops like Restasis (cyclosporine) and Xiidra (lifitegrast) can help. Restasis works by calming inflammation and slowly boosting your eye’s own tear production. But it takes months. Don’t expect relief in a week. Xiidra works faster-often in 2 to 4 weeks-and reduces the burning and grittiness by about 30%. Both require a prescription, and both cost hundreds of dollars a month. Insurance doesn’t always cover them, which is why many people stick with OTC options longer than they should.
If lubrication isn’t enough, punctal plugs might be the next step. These tiny, biocompatible devices block the tiny drains in your eyelids that let tears escape. Temporary collagen plugs last a few months and give you a test run. If you feel better, permanent silicone plugs can stay in for years. Clinical data shows they can increase tear volume by 40-50%. It’s not glamorous, but for some, it’s life-changing.
Lifestyle Changes That Actually Make a Difference
Medications don’t act alone. Your environment and habits either make dry eyes worse-or help them heal.First, humidity. Dry air pulls moisture from your eyes. If your home or office air is below 40% humidity, your tears evaporate faster. A simple humidifier set to 40-60% can cut tear evaporation by 25%. It’s cheaper than a bottle of drops and works while you sleep.
Screen time is another silent culprit. Staring at a computer or phone makes you blink 60% less. That’s why the 20-20-20 rule works: every 20 minutes, look at something 20 feet away for 20 seconds. People on antidepressants or antihistamines who follow this rule report 35% less eye strain.
Diet matters too. Omega-3 fatty acids-found in fish oil or algae supplements-help rebuild the oily layer of your tear film. Taking 1,000 to 2,000 mg of EPA and DHA daily improves tear stability in 60% of users within three months. It’s especially helpful if you’re on diuretics or other dehydrating meds.
Avoid direct airflow. Don’t sit in front of a fan, AC vent, or car heater blowing straight at your face. Air moving faster than 0.15 meters per second near your eyes increases evaporation by 30%. Rearrange your desk. Adjust your car vents. It’s a small change with a big payoff.
And quit smoking. Tobacco smoke irritates the eye surface and makes dry eye symptoms 45% worse. People who stop smoking notice improvement in just 2 to 4 weeks. No medication can match that kind of natural relief.

When to Talk to Your Doctor-And What to Ask
The biggest mistake people make? Keeping silent. They think dry eyes are just part of aging or screen use. But if you started a new medication and your eyes changed, it’s worth a conversation.Ask your doctor: “Could this drug be causing my dry eyes?” Then ask: “Is there an alternative with fewer eye side effects?” For example, some blood pressure meds like ACE inhibitors cause less dryness than beta-blockers. Some antidepressants like bupropion are less likely to cause dry eyes than SSRIs. Dose reduction helps too-in 55% of cases, lowering the dose improves symptoms without losing the drug’s benefit.
Never stop a medication cold turkey. Especially blood pressure pills, antidepressants, or heart meds. That can be dangerous. Work with your doctor and your eye specialist together. A coordinated plan is safer and more effective.
Real People, Real Results
One Reddit user on r/dryeye shared: “Three months on Zoloft, my eyes felt like sandpaper. My optometrist told me to switch to preservative-free Systane Ultra and do warm compresses twice a day. Two weeks later, I could read for more than 20 minutes without burning.”Another person on Accutane tried everything-drops, humidifiers, diet-until they got iLux thermal pulsation therapy. It costs $500 per session, but they got an 80% drop in symptoms. For some, that’s worth it.
But not everyone has access to expensive treatments. That’s why the basics matter so much: preservative-free tears, omega-3s, humidity, and avoiding airflow. These aren’t fancy. They’re practical. And they work for most people.
What to Avoid
Don’t use preserved drops more than four times a day. The preservatives build up and damage your cornea over time.Don’t apply eye drops right after your glaucoma meds. Wait 15 minutes. Otherwise, you’re washing out the treatment.
Don’t ignore persistent redness, pain, or vision changes. That’s not just dryness-it could be corneal damage. See an eye doctor.
And don’t assume your doctor knows this is a side effect. Most aren’t trained to connect dry eyes to meds unless you bring it up.
What’s Changing in 2025
The field is evolving. New preservative-free formulations are hitting the market faster. In 2023, 35% of artificial tears were preservative-free. That’s up from 15% just five years ago. The FDA now encourages drugmakers to remove toxic preservatives. And new diagnostic tools-like tear osmolarity tests and meibomian gland imaging-are helping doctors personalize treatment instead of guessing.There’s even a new cyclosporine formula called Cequa, using nanomicellar tech to deliver more drug with less irritation. Clinical trials for lipid-based emulsions targeting Accutane users are showing promising early results.
The message is clear: medication-induced dry eye is being taken seriously now. More doctors are screening for it. More patients are speaking up. And better tools are becoming available.
But the most powerful tool you have? Awareness. Know what you’re taking. Know how it might affect your eyes. And don’t suffer in silence.
Can dry eyes from medication be reversed?
Yes, in many cases. If the medication causing the dryness can be stopped, switched, or lowered, symptoms often improve within weeks to months. For example, switching from BAK-containing glaucoma drops to preservative-free versions reduces dryness by over 60%. Even with long-term meds like Accutane, symptoms can improve with proper lubrication, warm compresses, and omega-3s. Complete reversal depends on how much damage was done to the glands, but most people see significant relief with the right plan.
Are preservative-free artificial tears worth the cost?
If you’re using artificial tears four or more times a day, yes. Preserved drops contain chemicals that irritate your eyes over time, especially with frequent use. Preservative-free vials cost more per drop, but they’re safer for daily use. Many people find they need fewer drops overall because their eyes heal better without irritation. Some insurance plans cover them if prescribed. Even if you pay out of pocket, the long-term eye health benefit makes them a smart investment.
How long does it take for omega-3 supplements to help dry eyes?
Most people notice improvement in tear quality and reduced burning after 8 to 12 weeks of taking 1,000-2,000 mg of EPA and DHA daily. It takes time because omega-3s rebuild the lipid layer of your tears at a cellular level. Don’t expect overnight results. But studies show 60% of users have better tear stability after three months, especially those on dehydrating meds like diuretics.
Can I use eye drops with my contact lenses?
Only use drops labeled “for contact lens wearers.” Most artificial tears contain ingredients that can stick to lenses or cause clouding. Preservative-free single-use drops are often safe, but always check the label. Some people find switching to daily disposable lenses helps reduce irritation. If your eyes are very dry, your eye doctor might recommend wearing contacts fewer days a week or trying scleral lenses, which trap moisture under the lens.
What should I do if my dry eyes get worse after starting a new medication?
Don’t wait. Start using preservative-free artificial tears 4-6 times daily, begin warm compresses twice a day, and increase humidity. Then schedule an appointment with your eye doctor and your prescribing doctor. Bring a list of all your medications. Together, they can assess whether the drug is the likely cause and explore alternatives. Early action prevents long-term damage to your tear film and cornea.

