When your child gets a new prescription, the label might say 10 mL - but that’s not the dose. The real dose is 200 mg. Mixing up volume and medication amount is one of the most common - and dangerous - mistakes parents and even some providers make. A single error can mean a 2x, 3x, or even 5x overdose. And it’s not rare. According to the Institute for Safe Medication Practices, 56% of all pediatric medication errors are dosing mistakes. Most of them happen because the weight-based calculation wasn’t checked properly.
Why Pediatric Dosing Is Different
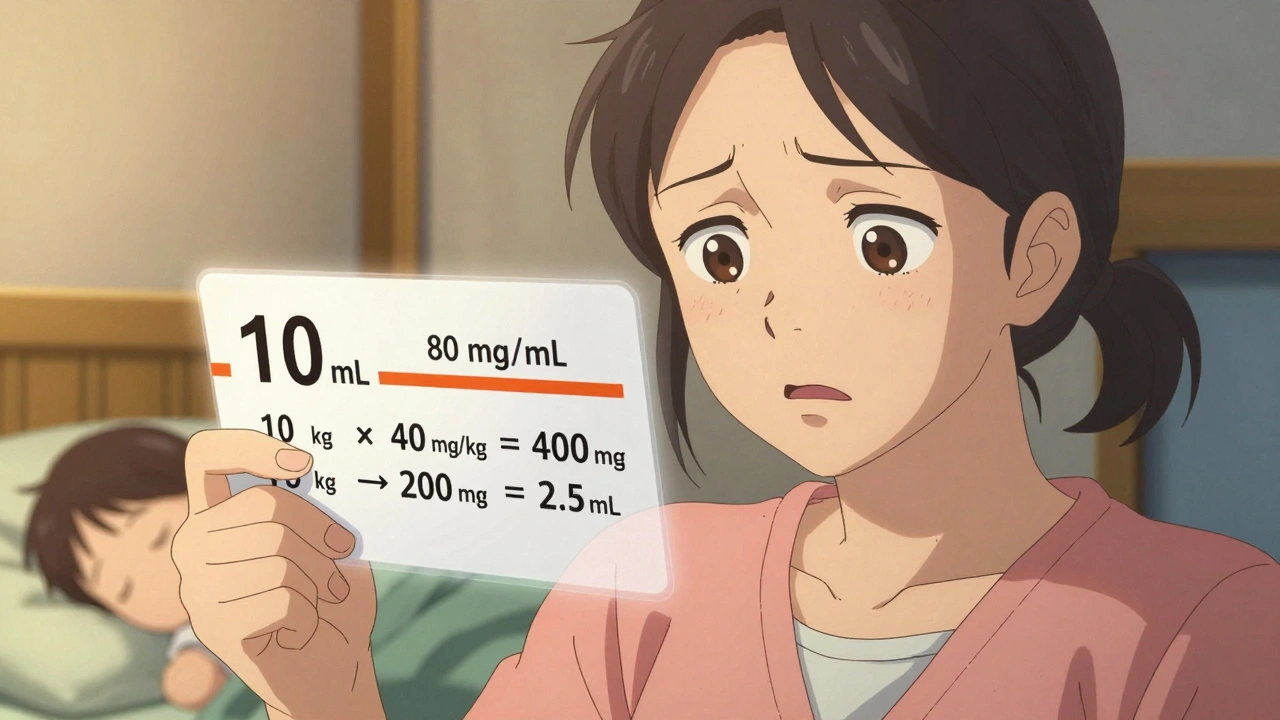
Children aren’t just small adults. Their bodies process medicine differently. A dose that’s safe for a 150-pound teen could be deadly for a 20-pound toddler. That’s why every pediatric prescription must be calculated by weight - not age, not guesswork, not adult dosing scaled down.The standard method is milligrams per kilogram (mg/kg). That means for every kilogram your child weighs, they get a specific number of milligrams of medicine. For example, amoxicillin for an ear infection might be 40 mg/kg per day, split into two doses. If your child weighs 10 kg, that’s 400 mg total per day - or 200 mg per dose.
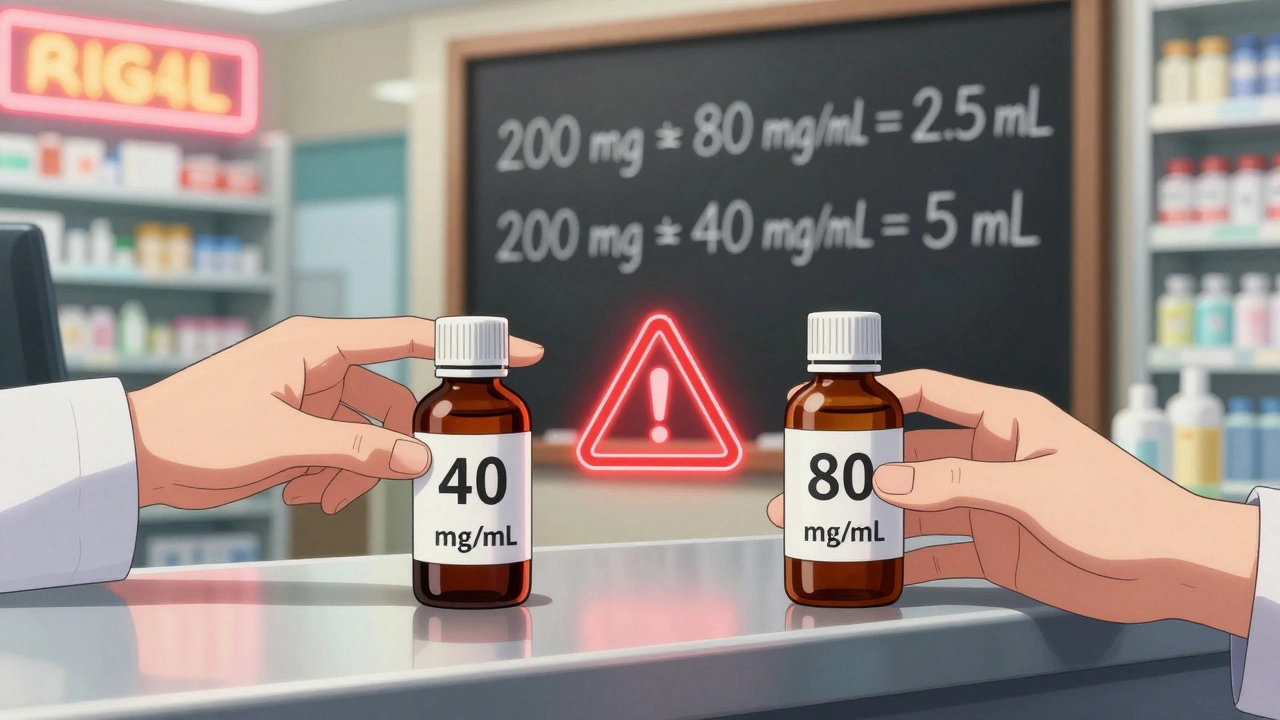
But here’s where things go wrong: the prescription might say “10 mL” on the label, and you assume that’s the dose. It’s not. The dose is the amount of medicine inside that volume. The concentration matters. Amoxicillin comes in different strengths - 40 mg/mL, 80 mg/mL, even 125 mg/mL. If you give 10 mL of the 80 mg/mL version when the dose was meant for 40 mg/mL, you’ve just given your child twice the intended dose.
What to Look for on the Prescription Label
A properly written pediatric prescription label must include three things:
- The child’s weight in kilograms (kg) - not pounds. If it says “22 lb,” that’s not enough. It should say “10 kg” (because 22 ÷ 2.2 = 10).
- The exact dose in milligrams (mg) - not just mL. Look for “200 mg” clearly written.
- The concentration - for example, “80 mg/mL” or “40 mg/mL.” This tells you how much medicine is in each milliliter.
If any of these are missing, call the pharmacy immediately. In 2022, the FDA issued new guidelines requiring all liquid pediatric medications to list both metric (mg/mL) and non-metric (teaspoon, tablespoon) measurements. But not all pharmacies are compliant yet. Don’t assume it’s there.
How to Verify the Dose Yourself
You don’t need to be a pharmacist to catch an error. Here’s how to check it step by step:
- Find the child’s weight in kg. If the label says “22 lb,” divide by 2.2. That’s 10 kg. If it says “10 kg,” great - you’re ahead.
- Find the ordered dose in mg/kg. The prescription should say something like “40 mg/kg/day.”
- Multiply weight × dose. 10 kg × 40 mg/kg = 400 mg total per day.
- Divide by how many times per day. If it’s twice daily, 400 mg ÷ 2 = 200 mg per dose.
- Check the concentration. If the bottle says “80 mg/mL,” then 200 mg = 2.5 mL. If it says “40 mg/mL,” then 200 mg = 5 mL.
- Compare to the label. Does the label say “200 mg” or just “2.5 mL”? If it only says “2.5 mL,” ask: “Is this 200 mg?”
One mother in Auckland caught a 2.5x overdose because she did this. Her child’s amoxicillin label said “10 mL.” She calculated the dose based on weight and realized it should’ve been 2.5 mL. She called the pharmacy. The pharmacist admitted they’d misread the concentration. “I almost gave my son a dangerous overdose,” she said. “I’m glad I checked.”
Common Mistakes That Lead to Overdoses
Here are the top three mistakes - and how to avoid them:
- Confusing mL with mg. This is the #1 error. “Give 10 mL” doesn’t tell you how much medicine is in there. Always ask: “What’s the dose in milligrams?”
- Wrong concentration. Amoxicillin comes in 80 mg/mL and 40 mg/mL. Giving the wrong one can double or halve the dose. Always check the bottle’s label for the concentration.
- Incorrect weight conversion. If the chart says “22 lb” and you guess “10 kg,” you’re close - but not exact. Use 1 kg = 2.2 lb. 22 ÷ 2.2 = 10. 25 ÷ 2.2 = 11.36. Don’t round unless instructed.
A 2022 study in the Journal of Pediatric Pharmacology and Therapeutics found that 18.7% of dosing errors came from weight conversion mistakes. That’s almost 1 in 5. Use a calculator. Write it down. Double-check.
What Pharmacists Should Do (And What You Can Ask For)
Best practice in hospitals and children’s pharmacies is dual verification. That means two people check the dose - one calculates, the other confirms. But in community pharmacies, that’s not always standard.
Ask your pharmacist: “Can you show me how you calculated this dose?” or “Can you confirm the dose is 200 mg based on my child’s weight of 10 kg?” Most will be happy to walk you through it. If they get defensive, that’s a red flag.
Pharmacists are trained to catch these errors. But if you don’t ask, they might assume you understand. Don’t assume. Always verify.
Technology Can Help - But Don’t Rely on It Alone
Hospitals use systems like EPIC and Cerner that automatically flag incorrect doses. They can catch 94% of calculation errors. But community pharmacies? Many still use older systems. Even if the system flags a dose, it’s not foolproof.
AI tools like DoseSpot’s Pediatric Safety Module are now being used in some clinics. They cross-check weight, age, and drug against 15,000+ guidelines. Accuracy? 99.2%. But if you’re picking up a prescription at a local pharmacy, don’t assume they’re using this tech.
Technology helps - but your eyes and questions are still the most reliable safety net.
What to Do If You’re Unsure
If anything feels off - the dose seems too small, too big, or the label is unclear - do this:
- Call the prescribing doctor’s office.
- Call the pharmacy and ask them to recheck the calculation.
- Use the FDA’s free Safe Use of Pediatric Liquid Medicines guide (available online) to cross-check typical doses.
- Take a photo of the label and show it to another parent or healthcare worker you trust.
There’s no such thing as asking too many questions when it comes to your child’s medicine.

Real Stories, Real Risks
A mother in Wellington found her 18-month-old’s acetaminophen label said “10 mL.” She thought it was the standard 160 mg/5 mL concentration. But the bottle was actually 80 mg/0.8 mL - a much stronger concentration. She’d have given 1,000 mg instead of 160 mg. That’s a toxic dose. She caught it because she compared the label to the manufacturer’s dosing chart.
Another parent in Christchurch saw a prescription for “15 mL” of amoxicillin for her 2-year-old. She did the math: 12 kg × 40 mg/kg = 480 mg total. The concentration was 40 mg/mL, so 480 mg = 12 mL. The label said 15 mL - 3 mL too much. She called the pharmacy. They corrected it.
These aren’t hypotheticals. These are real events. And they’re preventable.
Final Checklist Before Giving Any Pediatric Medicine
Before you give your child any liquid medicine, run through this:
- ✅ Is the child’s weight listed in kg?
- ✅ Is the dose written in mg - not just mL?
- ✅ Is the concentration (mg/mL) clearly printed on the bottle?
- ✅ Did you calculate: weight (kg) × dose (mg/kg) = total mg per day?
- ✅ Did you divide by frequency (e.g., twice daily)?
- ✅ Did you use the concentration to convert mg → mL? (Total mg ÷ mg/mL = mL)
- ✅ Does the volume on the label match your calculation?
If you can answer “yes” to all seven, you’ve done more than most. You’ve protected your child.
What if the prescription only says mL and not mg?
If the label only shows volume (like 5 mL) and doesn’t state the dose in milligrams, ask the pharmacist: “What is the exact amount of medicine in milligrams?” Never assume. A dose written as “10 mL” without mg is incomplete and potentially dangerous. The FDA and American Academy of Pediatrics require both to be listed. If they can’t provide it, do not give the medicine until you get clarification.
Can I use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary in size and can be off by 20-50%. Always use the measuring device that comes with the medicine - a syringe or oral dosing cup. If one isn’t included, ask the pharmacy for one. A 5 mL dose with a kitchen teaspoon might end up being 7 mL. That’s a 40% overdose.
Why is weight in kg better than pounds for dosing?
All medical dosing guidelines for children are based on kilograms. The conversion from pounds to kilograms (1 kg = 2.2 lb) is standardized globally in medicine. Using pounds increases the chance of rounding errors or miscommunication. For example, 25 lb is 11.36 kg - not 11 or 12. Precision matters. Most hospitals now require weight to be entered in kg during registration.
What should I do if I think I gave the wrong dose?
Call your doctor or poison control immediately. In New Zealand, call Poison Control at 0800 764 766. Do not wait for symptoms. Even if your child seems fine, some overdoses take hours to show signs. Keep the medicine bottle and label handy - they’ll need the concentration and exact dose you gave.
Are there apps that can help me check pediatric doses?
Yes. Apps like Epocrates, Lexicomp, and DoseSpot have pediatric dosing calculators built in. Some are free. Enter the child’s weight, the drug name, and the concentration - the app will calculate the correct dose. But don’t rely on them alone. Always cross-check with the prescription label and ask your pharmacist to confirm. Apps can have outdated data or incorrect defaults.
Next Steps for Parents and Caregivers
Start today: Write down your child’s current weight in kg and keep it on your phone or in your wallet. The next time you get a prescription, you’ll have it ready. Make it a habit to ask for the dose in mg - not just mL. Show the label to another adult before giving the medicine. If you’re ever unsure, call the pharmacy. No question is too small.
Medication safety isn’t just the doctor’s job. It’s yours too. And when you know how to check the dose, you’re not just following instructions - you’re protecting your child.