When your blood calcium stays too high for too long, your body starts breaking down. Not from overdoing it at the gym or eating too much dairy-this is something deeper. It’s called hyperparathyroidism, and it’s quietly stealing calcium from your bones, clogging your kidneys, and fogging your brain-all because one or more tiny glands in your neck won’t stop sending the wrong signal.
What’s Really Going On Inside Your Body?
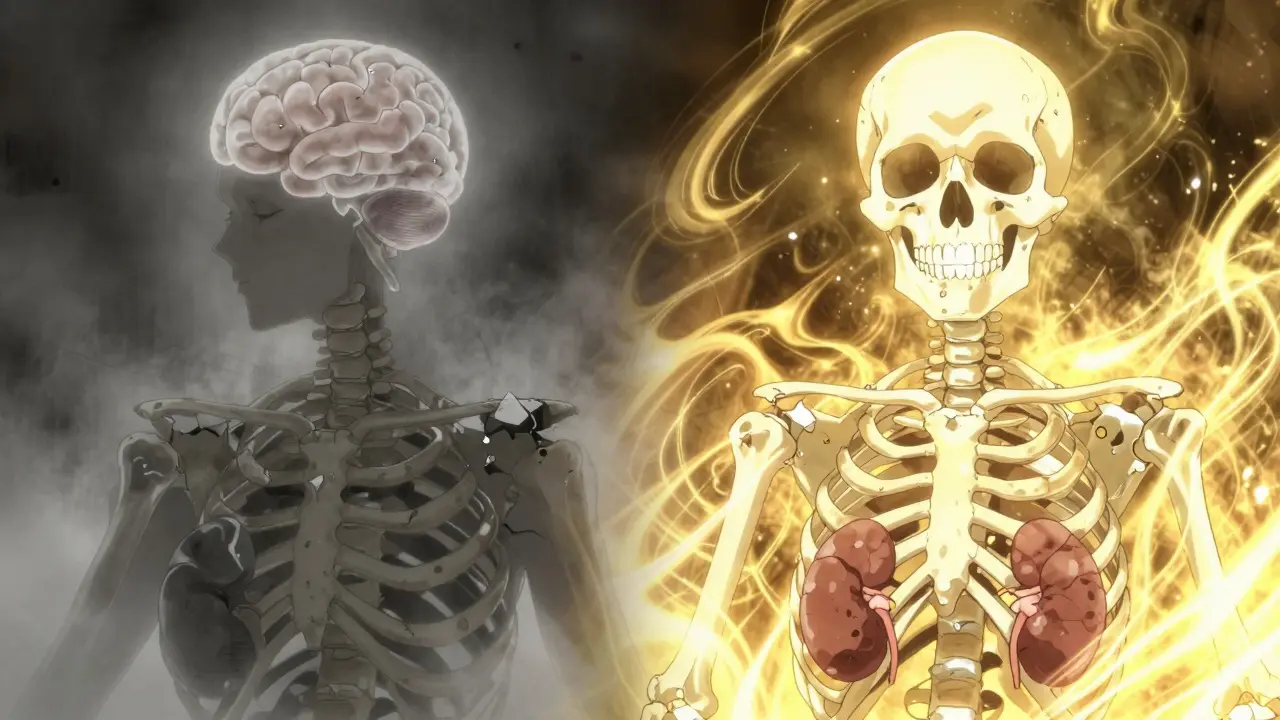
Your parathyroid glands are four pea-sized organs behind your thyroid. They don’t make thyroid hormones. Instead, they control calcium-the mineral that keeps your bones strong, your nerves firing, and your muscles contracting. Normally, when calcium drops, these glands release parathyroid hormone (PTH) to pull calcium from your bones, boost absorption from food, and tell your kidneys to hold onto more. Simple. Balanced. In hyperparathyroidism, that system breaks. One gland (usually) starts pumping out too much PTH, even when your calcium is already sky-high. It’s like a thermostat stuck on ‘heat’ while your house is already boiling. The result? Calcium levels climb past 10.5 mg/dL (normal is 8.5-10.2). That’s not just a lab number-it’s a red flag. This isn’t just about calcium floating around. It’s about what that excess calcium does to your body. Your bones lose density at 2-4% per year. Your kidneys start forming stones. Your muscles feel weak. You get tired all the time. Some people describe it as ‘brain fog’-like your thoughts are wrapped in cotton. And if left unchecked, your risk of breaking a hip or spine jumps by 30-50%.Why Do Some People Get This and Others Don’t?
About 100,000 Americans are diagnosed with primary hyperparathyroidism each year. Women are three times more likely to get it than men. African Americans have higher rates too. Most cases happen after age 50, but it can strike younger people-especially if there’s a family history. In 85% of cases, it’s caused by a benign tumor called an adenoma on one parathyroid gland. In 15%, all four glands swell up (hyperplasia). Less than 1% are cancerous. The exact trigger? No one knows for sure. It’s not caused by diet, stress, or lifestyle. It’s a biological glitch-often random, sometimes inherited. There are other types, too. Secondary hyperparathyroidism happens when your kidneys fail and your calcium drops, so your glands overwork to compensate. Tertiary happens after a kidney transplant-your glands get so used to overproducing that they keep going even when calcium returns to normal. But 80-85% of cases are primary. That’s the one that needs serious attention.How Do You Know If You Have It?
Most people don’t feel symptoms at first. That’s why it’s often found by accident-during a routine blood test for something else. But if you’ve had unexplained fatigue, bone pain, frequent kidney stones, or trouble concentrating, it’s worth asking your doctor to check your calcium and PTH levels. A diagnosis needs two things: elevated calcium on two separate blood tests (at least a week apart), and PTH that’s either high or ‘inappropriately normal.’ That last part is tricky. If your calcium is 11.2 but your PTH is 60 (right at the top of normal), that’s still too high. Your glands should be shutting down, not staying active. Imaging comes next. A sestamibi scan (a nuclear medicine test) finds the bad gland in 90% of cases. Ultrasound helps too. For complex cases, a 4D-CT scan gives a 95% accuracy rate. These aren’t just fancy pictures-they’re essential. Surgery only works if the surgeon knows exactly where to look.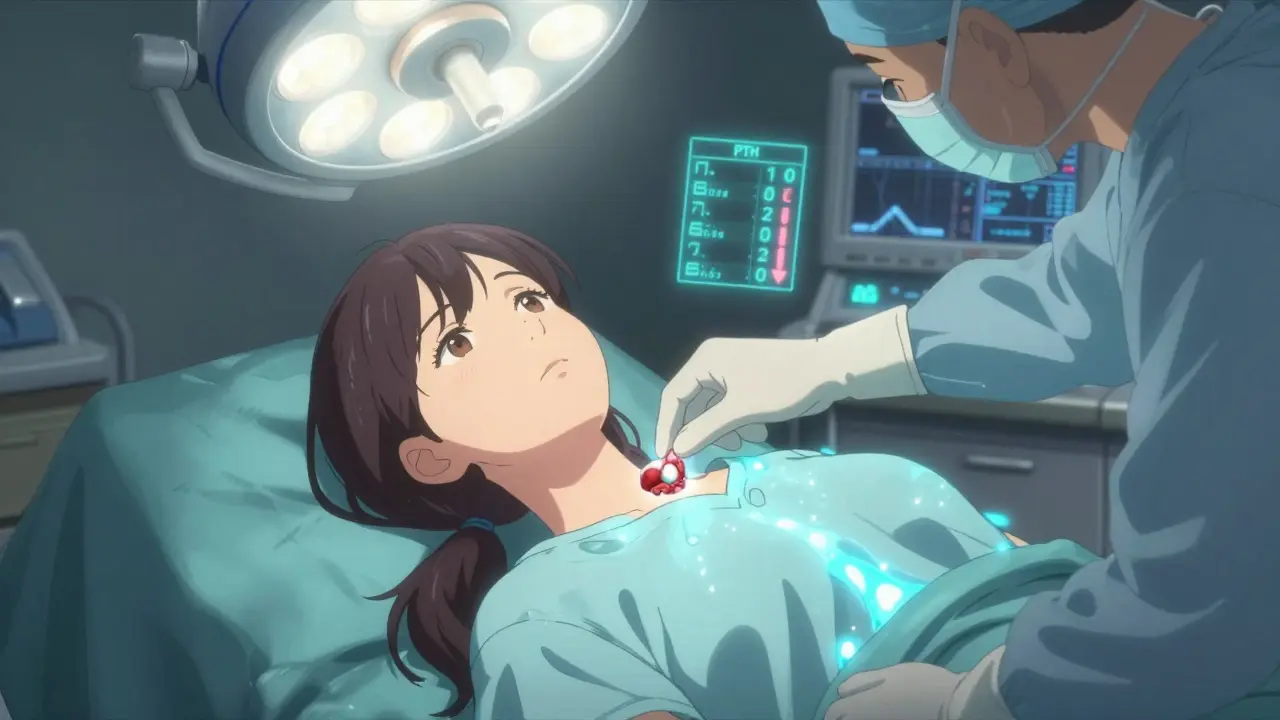
Is Surgery the Only Real Solution?
Yes. And it’s not just the best option-it’s the only one that cures it. Medications like cinacalcet or bisphosphonates can help manage symptoms or slow bone loss, but they don’t fix the root problem. They’re temporary fixes for people who can’t have surgery. For everyone else, removing the faulty gland(s) is the answer. Minimally invasive parathyroidectomy is now the standard. A small incision, a 1-2 hour operation, and most people go home the same day. Success rates? 95-98% for single-gland disease. The surgeon uses real-time PTH monitoring: if the hormone drops by more than 50% within 10 minutes of removing the gland, you’re cured. Recovery is quick. Most people feel better in days. Bone pain fades. Energy returns. Kidney stones become rare. One patient on a support forum said, ‘After seven years of being told I was depressed, my brain felt like someone turned the lights back on.’What Happens After Surgery?
Your body needs time to adjust. For 2-8 weeks, you might feel tingling in your fingers or lips. That’s not a complication-it’s a sign your body is rebalancing. Your calcium levels drop temporarily because your bones start sucking calcium back in. That’s a good thing. It means your skeleton is healing. You’ll need calcium supplements (500-1000 mg three times a day) and sometimes vitamin D (calcitriol) for a few weeks. Most people stop them within two months. Your doctor will check your calcium at 4, 24, and 72 hours after surgery to make sure you’re not dipping too low. Bone density starts improving within a year. On average, your spine gains 3-5% density in the first year and 5-8% by year two. That’s not just a number-it’s fewer fractures, less pain, more mobility.Who Should Have Surgery?
The 2022 international guidelines say surgery is recommended if you have:- Calcium more than 1 mg/dL above the upper limit of normal
- Reduced kidney function (creatinine clearance under 60 mL/min)
- Bone density T-score of -2.5 or lower (osteoporosis)
- Age under 50
What If You Don’t Want Surgery?
Some people choose monitoring instead. That’s okay-if you meet strict criteria: calcium under 11 mg/dL, normal kidney function, no osteoporosis, and over 50 years old. You’ll need yearly blood tests, DXA scans every 1-2 years, and to avoid thiazide diuretics (which worsen high calcium) and excessive vitamin D. But here’s the catch: 15-20% of people who avoid surgery end up with complications later. And if your calcium was above 12 mg/dL before surgery, you’re more likely to still feel tired or foggy even after the gland is removed. Prolonged exposure to high calcium can cause lasting changes.What’s New in 2025?
New tools are making diagnosis faster and surgery safer. In 2024, the FDA approved etelcalcetide for primary hyperparathyroidism-a drug that slashes PTH by 45% in trials. It’s not a cure, but it’s a lifeline for people who can’t have surgery. AI is helping too. New algorithms analyze sestamibi scans and ultrasounds together, cutting false positives by 35%. That means fewer unnecessary surgeries and better targeting of the problem gland. And the success rate? It’s never been higher. Surgeons who do more than 50 parathyroid operations a year have a 98% cure rate. That’s why finding a high-volume center matters. Don’t settle for a general surgeon. Look for someone who specializes in endocrine surgery.What You Can Do Now
If you’ve been told your calcium is high, don’t wait. Get your PTH checked. Ask for a sestamibi scan. Talk to an endocrine surgeon-even if you’re not sure about surgery yet. Knowledge is power. In the meantime:- Drink plenty of water-helps flush excess calcium
- Get daily weight-bearing exercise (walking, lifting weights)
- Don’t take calcium supplements unless prescribed
- Avoid thiazide diuretics (like hydrochlorothiazide) if you can
- Keep your vitamin D levels in check-deficiency makes PTH worse

