Many people turn to kava as a natural way to ease anxiety or get a calm, relaxed feeling. But if you’re taking any sedative medication-like Xanax, Valium, lorazepam, or even sleep aids-combining it with kava can be dangerous. The risks aren’t just about feeling extra sleepy. There’s a real chance of serious liver damage, and the effects can sneak up on you without warning.
How Kava Works in Your Body
Kava comes from the roots of the Piper methysticum plant, traditionally used in Pacific Island cultures for ceremonies and relaxation. Its active compounds, called kavalactones, cross the blood-brain barrier quickly-within 15 minutes-and start affecting your central nervous system. You’ll feel a sense of calm, muscle relaxation, and mild sedation, usually peaking around 90 minutes after taking it. Unlike alcohol, kava doesn’t impair coordination as much, but it still slows down brain activity.
Traditional water-based kava drinks, made the way Pacific Islanders prepare them, contain about 150-250 mg of kavalactones per serving. But commercial supplements? Those can pack in up to 300 mg per pill or capsule, often extracted with alcohol or acetone. That’s a big difference. These concentrated forms are what most liver damage reports are tied to.
The Liver Risk: It’s Real and Often Overlooked
The U.S. Food and Drug Administration (FDA) issued a warning about kava back in 2002, after more than two dozen cases of severe liver injury were reported worldwide. Some people needed liver transplants. Even though kava is still sold as a dietary supplement in the U.S., it’s banned as a medicinal product in the EU, Canada, the UK, and Switzerland because of these risks.
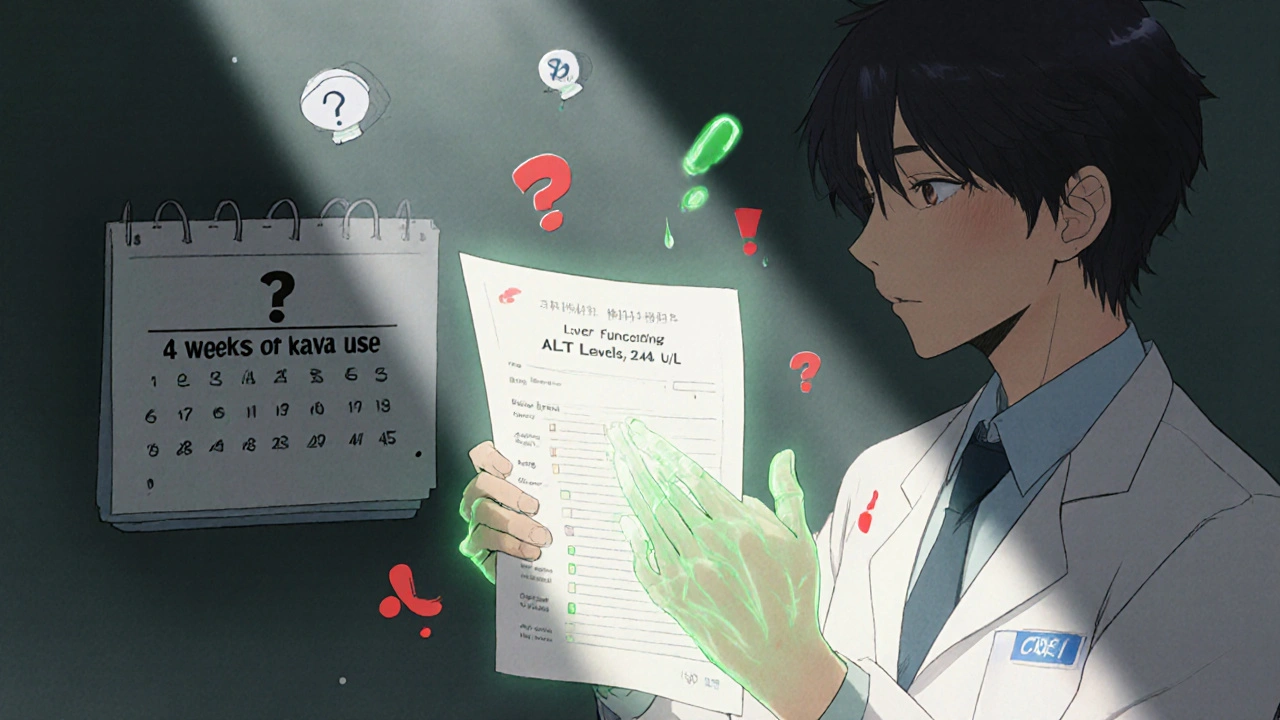
Here’s what’s scary: liver damage from kava doesn’t always show up right away. It can take weeks or months. Early signs-fatigue, nausea, dark urine, yellowing of the skin or eyes-are easy to ignore. By the time someone gets tested, their liver enzymes (like ALT) are already sky-high. One Sacramento County case from 2023 showed a patient with ALT levels at 2,840 U/L (normal is under 40). That’s liver failure territory.
Why does this happen? Scientists aren’t 100% sure, but kava seems to interfere with liver enzymes (CYP2D6, CYP2C9, CYP3A4) that break down medications and toxins. When those enzymes get blocked, drugs build up in your system-and your liver gets overwhelmed.
Why Mixing Kava with Sedatives Is a Bad Idea
If you’re on benzodiazepines, barbiturates, sleep pills, or even some antidepressants that cause drowsiness, adding kava is like pouring gasoline on a fire. The effects aren’t just added-they’re multiplied.
Studies show kava can increase the blood levels of midazolam (a sedative) by 27%. That means a normal dose of your prescription could act like a double dose. People have reported being unable to stand for hours, slurring speech, or passing out after combining kava with lorazepam or diazepam. One Reddit user described being “confused and stuck on the couch” for eight hours after taking kava with their prescribed 0.5 mg lorazepam.
The FDA’s adverse event database has 37 reports of excessive sedation linked to kava, with 12 cases requiring emergency care. And it’s not just about feeling sleepy. The combination can lead to dangerously low breathing rates, especially in older adults or people with existing lung or heart conditions.
Who’s Most at Risk?
Not everyone who takes kava gets hurt. But some groups are far more vulnerable:
- People taking any CNS depressant (sleep meds, anti-anxiety drugs, muscle relaxants)
- Those with pre-existing liver disease (hepatitis, fatty liver, cirrhosis)
- People who use kava daily for more than a few weeks
- Those taking high-dose supplements (over 250 mg kavalactones daily)
- Anyone who drinks alcohol while using kava-this combo raises liver damage risk even more
Australia’s Therapeutic Goods Administration says the risk of liver injury is “very low but not negligible”-but that’s only if you’re using traditional, low-dose kava. Commercial extracts? The risk jumps.
What the Experts Say
There’s disagreement among researchers, but the consensus is clear: don’t take kava with sedatives.
Dr. Jay H. Hoofnagle, who runs LiverTox at the NIH, says at least a dozen cases of acute liver failure have been directly linked to kava. He points to the fact that many patients had no other known causes of liver damage-just kava and medication.
On the other hand, some argue that past cases might have been caused by contaminated products or other factors. But even if kava isn’t the sole culprit, it’s clearly a major contributor. The European Food Safety Authority says there’s no safe level of kava use if you’re on medications metabolized by CYP2D6, CYP2C9, or CYP3A4. That covers most sedatives, antidepressants, and painkillers.
And here’s something most people don’t realize: only 22% of patients with liver problems voluntarily tell their doctors they’re using kava. Doctors don’t always ask. Pharmacists don’t always check. You have to bring it up.
What Should You Do?
If you’re using kava and taking sedative medication:
- Stop immediately. Don’t wait for symptoms. The damage can be silent until it’s too late.
- Get your liver checked. Ask your doctor for a liver function test (ALT, AST, bilirubin). Even if you feel fine, it’s worth knowing.
- Talk to your prescriber. If you’re using kava for anxiety, ask about safer alternatives. Buspirone, SSRIs, or therapy have proven track records without the liver risk.
- Don’t assume “natural” means safe. Kava isn’t regulated like medicine. Two bottles labeled “kava extract” can have wildly different kavalactone levels.
If you’re not on sedatives but still want to try kava:
- Stick to traditional water-based preparations (not alcohol extracts)
- Limit yourself to 70 mg kavalactones per day or less
- Don’t use it daily for more than 4 weeks
- Get liver tests every 4-6 weeks if you use it regularly
- Never mix with alcohol
What’s Changing in 2025?
The FDA is pushing for stricter oversight of botanical supplements. In 2023, they gave $2.4 million to Oregon State University to study whether “noble” kava varieties-used in Pacific traditions-are safer than the commercial “two-day” types. Early results suggest they might be.
Meanwhile, states are stepping in. California issued formal warnings in May 2024. New York is considering a law requiring liver toxicity labels on all kava products. Sales are already dropping-22% fewer kava supplements are expected to be sold by 2026, according to the Global Wellness Institute.
But here’s the twist: traditional kava bars are still growing. In the U.S., there are 312 of them as of early 2024. These places serve water-based kava, often in ceremonial settings, with no concentrated extracts. For now, that’s the safest way to experience kava-if you’re not on meds.
Final Thoughts
Kava isn’t inherently evil. It’s been used safely for centuries in the Pacific. But when you mix it with modern sedative medications, you’re playing with fire. The liver doesn’t warn you. The sedation doesn’t always show up right away. And once damage is done, it’s not always reversible.
If you’re taking any medication that makes you drowsy, don’t take kava. Period. If you’re using kava for anxiety and want to stop your prescription, talk to your doctor first-don’t just swap one for the other.
Your body doesn’t care if something is “natural.” It only cares about what’s in your bloodstream. And right now, the evidence is clear: kava and sedatives don’t mix.
Can kava cause liver damage even if I don’t take any medications?
Yes. While the risk is much higher when combined with sedatives or alcohol, there are documented cases of liver injury in people who took kava alone. Most of these cases involved high-dose supplements (over 250 mg daily) used for more than a few weeks. Traditional water-based kava has a much lower risk, but it’s not zero. The FDA and European regulators agree: no level of kava use can be declared completely safe for the liver.
Is kava safer than prescription anxiety meds?
No, not when you look at the full picture. Prescription anxiolytics like alprazolam have a documented liver injury rate of about 1 in 100,000 prescriptions. Kava’s estimated rate is lower-less than 1 in 1,000,000 daily doses-but that number is likely underreported. The bigger issue is control: prescription drugs have standardized doses, known side effects, and strict monitoring. Kava doesn’t. You don’t know how much kavalactone is in your supplement, and there’s no oversight. That unpredictability makes it riskier.
What are the signs of kava-related liver damage?
The earliest signs are often subtle: unexplained fatigue, loss of appetite, nausea, dark urine, or light-colored stools. As it progresses, you may notice jaundice (yellow skin or eyes), itching, or swelling in the abdomen. These symptoms usually appear 1 to 4 months after starting kava. If you’ve been using kava and notice any of these, stop immediately and get a liver function test. Waiting can be life-threatening.
Can I use kava if I’m on a low dose of a sedative?
No. Even low doses of sedatives-like 0.5 mg of lorazepam or 5 mg of diazepam-can interact dangerously with kava. The liver enzymes that break down both substances get overwhelmed. The sedative effect can become unpredictable and potentially life-threatening. There’s no safe threshold for combining them. If you’re on any CNS depressant, avoid kava completely.
What’s the safest way to take kava if I’m not on meds?
If you choose to use kava, stick to traditional water-extracted preparations served in kava bars or made at home with noble kava root. Avoid capsules, tinctures, or alcohol-based extracts. Limit intake to 70 mg kavalactones per day, use it no more than 2-3 times per week, and never for longer than 4 weeks without a break. Get liver tests every 6 weeks. And never mix with alcohol or other sedatives.

