Bone Marrow Suppression Symptom Checker
Symptom Assessment
Answer the following questions about your symptoms. This tool helps you understand if you might be experiencing bone marrow suppression related to medications.
Results
When you take a medication to treat cancer, an autoimmune disease, or even a stubborn infection, you expect it to help. But for many people, one of the most dangerous side effects isn’t nausea or hair loss-it’s something you can’t see: bone marrow suppression. This isn’t just a lab result. It’s when your body stops making enough blood cells, leaving you vulnerable to infections, fatigue, and bleeding. And it’s more common than most people realize.
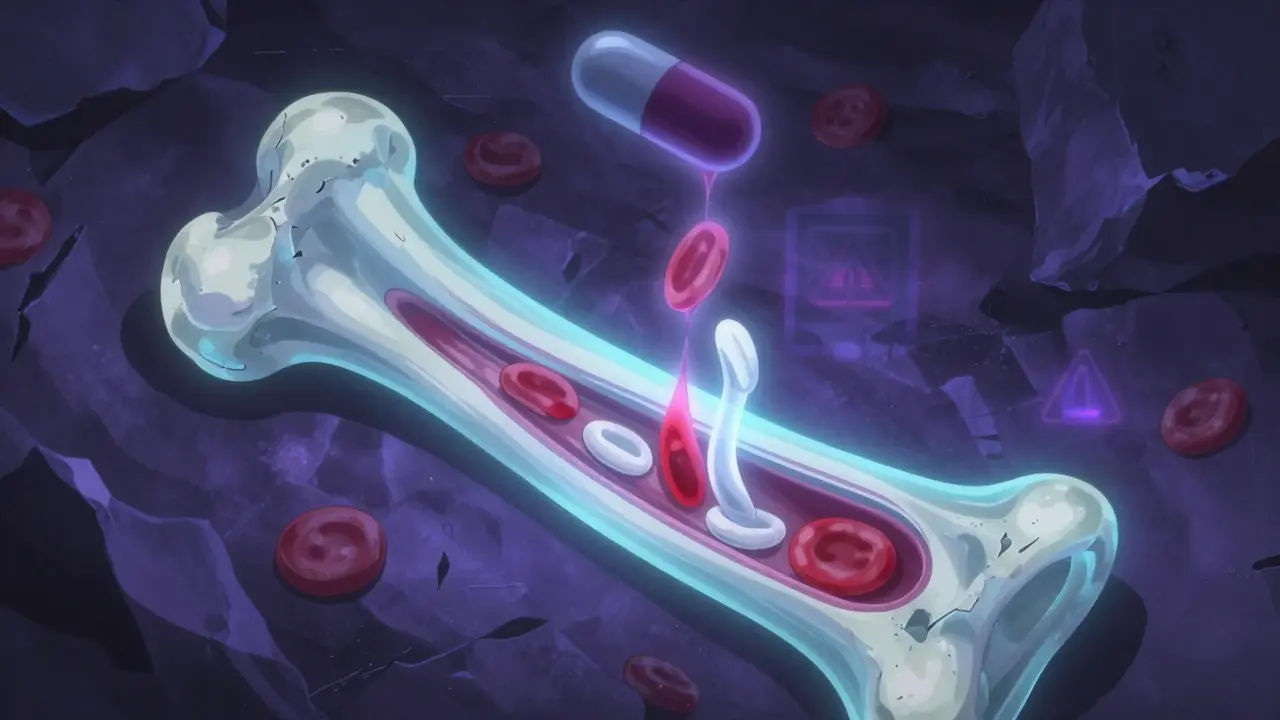
What Exactly Is Bone Marrow Suppression?
Your bone marrow is the soft tissue inside your bones. It’s where all your blood cells are made: red cells that carry oxygen, white cells that fight infection, and platelets that stop bleeding. When medications damage this system, your body can’t keep up with demand. That’s bone marrow suppression-or myelosuppression. It’s not a disease. It’s a reaction. And it can happen with drugs you might not expect.Chemotherapy is the biggest culprit. About 70 to 80% of people on standard cancer treatments will experience some level of suppression. But it’s not just chemo. Antibiotics like trimethoprim-sulfamethoxazole, immunosuppressants like azathioprine, and even some antivirals can trigger it. The effect isn’t immediate. It usually hits 7 to 14 days after starting treatment, when blood counts drop to their lowest point-the nadir.
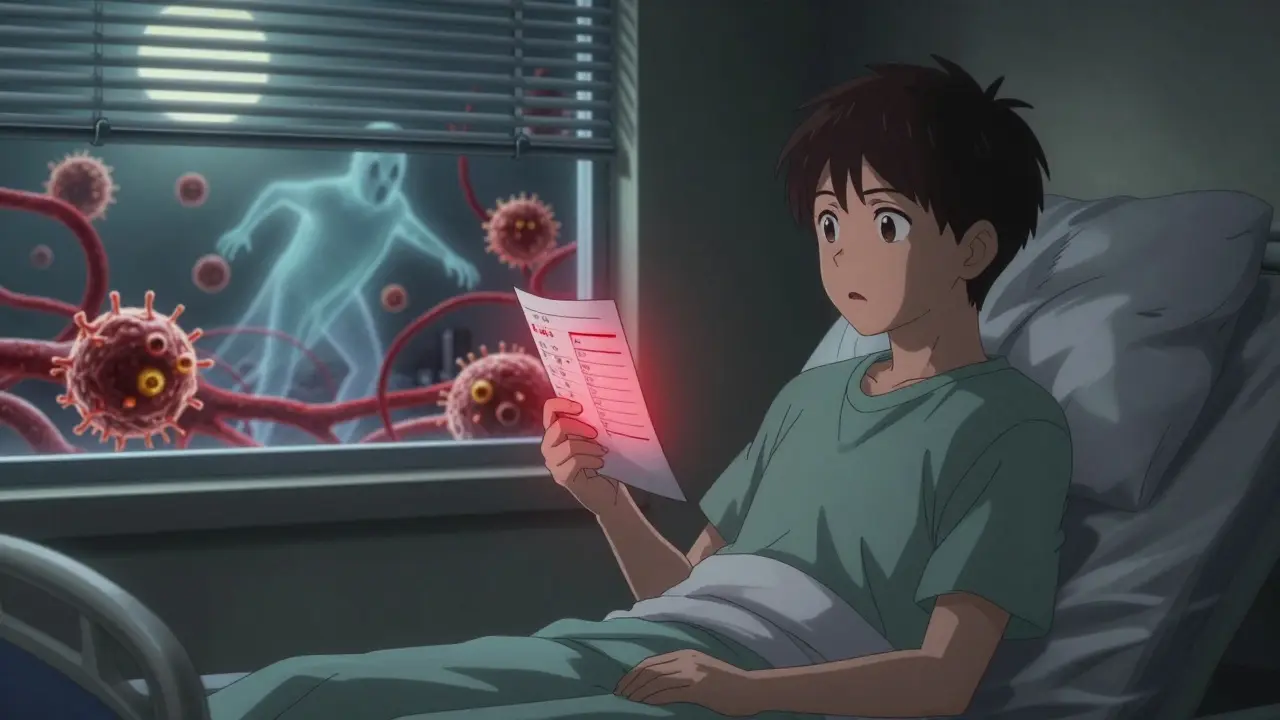
How Do You Know If Your Blood Counts Are Low?
You won’t always feel it at first. But as counts drop, symptoms show up:- Neutropenia (low white cells): Fever over 38.3°C (101°F), sore throat, mouth sores, or just feeling unusually tired. A count below 1,500 cells/μL is considered low; below 500 is dangerous.
- Anemia (low red cells): Constant fatigue, dizziness, pale skin, shortness of breath even walking up stairs. Hemoglobin below 13.5 g/dL in men or 12.0 g/dL in women signals trouble.
- Thrombocytopenia (low platelets): Easy bruising, nosebleeds, bleeding gums, tiny red dots on the skin (petechiae). Counts below 150,000/μL are low; below 50,000/μL raise bleeding risk.
These aren’t vague symptoms. They’re red flags. A simple blood test-a complete blood count, or CBC-can catch them early. Most oncology teams check CBCs weekly during active treatment. For high-risk patients, like those on carboplatin, counts are tracked even more closely. Carboplatin alone causes severe thrombocytopenia in 30 to 40% of patients at standard doses.
Which Medications Are Most Likely to Cause It?
Not all drugs are equal when it comes to bone marrow damage. Here’s what the data shows:- Chemotherapy drugs: Especially platinum-based agents like carboplatin and cisplatin, alkylators like cyclophosphamide, and nucleoside analogs like fludarabine. Fludarabine causes prolonged lymphopenia in 65% of chronic lymphocytic leukemia patients.
- Immunosuppressants: Azathioprine, used for organ transplants and autoimmune diseases, suppresses bone marrow in 5 to 10% of users. In those cases, switching to mycophenolate mofetil restores blood counts in 78% of patients within 4 to 6 weeks.
- Antibiotics and antivirals: Trimethoprim-sulfamethoxazole (Bactrim), chloramphenicol, and some HIV drugs can trigger suppression, especially with long-term use.
- Newer targeted therapies: Even drugs designed to be gentler can have hidden effects. Some kinase inhibitors and monoclonal antibodies are now known to cause cytopenias.
The key isn’t just the drug-it’s the dose, the duration, and your body’s unique response. Some people get hit hard with low doses. Others tolerate high doses fine. That’s why personalized monitoring matters.
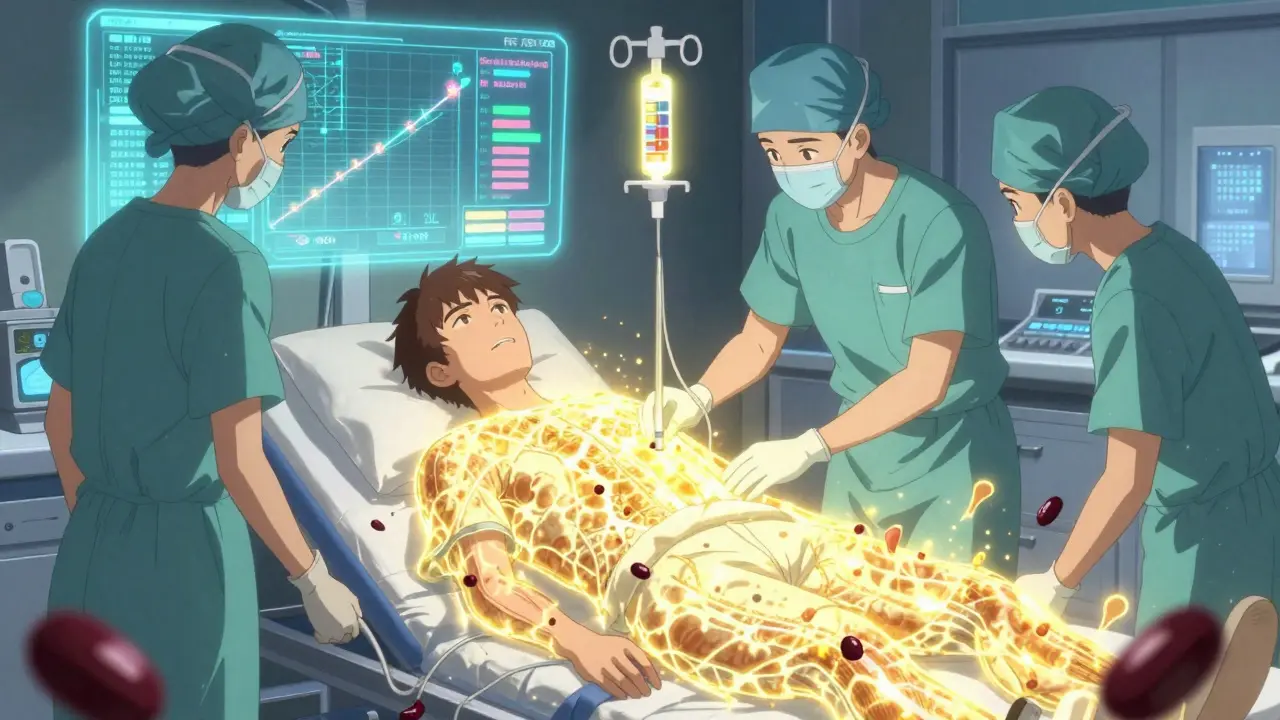
How Is It Treated?
Treatment depends on how bad it is. Mild cases (Grade 1-2) often just need watchful waiting and maybe a small dose reduction. But severe cases (Grade 3-4) demand action.For low white blood cells, doctors often turn to growth factors like filgrastim (Neupogen) or pegfilgrastim (Neulasta). These drugs stimulate the bone marrow to make more neutrophils. Studies show they cut the duration of neutropenia by an average of 3.2 days. That might sound small, but it means fewer hospital visits, fewer infections, and fewer delays in cancer treatment.
There’s a newer option: trilaciclib (Cosela). Approved by the FDA in 2021, it’s the first drug designed to protect the bone marrow before chemotherapy starts. In clinical trials, it reduced myelosuppression by 47% in small cell lung cancer patients. It’s given as an IV infusion right before chemo-like a shield.
For low red blood cells, transfusions are used when hemoglobin drops below 8 g/dL. For platelets, transfusions kick in when counts fall below 10,000/μL-or if there’s active bleeding. These aren’t cures. They’re stopgaps. But they keep people alive and out of the ER.
In rare cases where suppression doesn’t improve-even after stopping the drug-stem cell transplantation becomes an option. Success rates with matched sibling donors are 65 to 75%, according to the Center for International Blood and Marrow Transplant Research.
What Patients Are Really Experiencing
Behind the numbers are real people. A 2022 survey of 1,245 cancer patients found that 74% had treatment delayed because of low blood counts. Another 68% said they lived in constant fear of infection during neutropenic periods. On online forums, patients praise pegfilgrastim for keeping them on track-but complain bitterly about the cost. In the U.S., a single Neulasta shot can cost $6,500 out of pocket.One Reddit user on r/cancer wrote: “I had to stop carboplatin after three rounds because my platelets kept crashing. My oncologist said I’d need a transfusion every two weeks. I couldn’t do it.” That’s not rare. In fact, 41% of patients in a 2022 ASCO survey quit treatment entirely because of persistent bone marrow suppression.
It’s not just about the drugs. It’s about quality of life. Missing work. Canceling family events. Avoiding public places. That’s the hidden cost of suppression.
How to Manage It Daily
If you’re on a myelosuppressive drug, here’s what you need to do:- Check your temperature daily. Any fever over 38.3°C (101°F) is an emergency. Call your doctor immediately. Neutropenic fever can turn deadly in hours.
- Avoid crowds and sick people. Even a common cold can be dangerous if your white cells are low.
- Use a soft toothbrush and electric razor. No flossing hard. No shaving with a blade. Bleeding risks are real.
- Don’t take NSAIDs like ibuprofen. They thin the blood. Acetaminophen is safer for pain or fever.
- Know your CBC numbers. Keep a log. If your platelets drop below 50,000 or your neutrophils below 1,000, talk to your team about growth factors.
For pediatric patients, hospitals like Children’s Hospital of Philadelphia monitor ANC every 48 to 72 hours during chemo cycles. Growth factors start when ANC dips below 1,000. That’s aggressive-but it works.
What’s Changing in 2025?
The field is moving fast. In May 2023, the FDA approved lixivaptan as an adjunct therapy, cutting transfusion needs by 31% in trials. At the 2023 American Society of Hematology meeting, magrolimab showed a 54% drop in transfusion-dependent anemia for myelodysplastic syndrome patients.But the biggest shift is in prevention. Doctors are no longer waiting for counts to crash. They’re using genetic testing to predict risk. A 2023 study in Nature Medicine found that people with TP53 mutations are 3.7 times more likely to develop severe suppression. That means some patients can be offered protective drugs like trilaciclib before they even start chemo.
By 2027, experts predict 70% of high-risk cases will use prophylactic strategies-preventing suppression before it starts, not fixing it after.
What You Should Ask Your Doctor
Don’t wait for symptoms. Ask these questions upfront:- “Which of my medications can lower my blood counts?”
- “How often will you check my CBCs?”
- “What’s my risk for severe suppression based on my treatment plan?”
- “Are there protective drugs like trilaciclib or growth factors I should consider?”
- “What signs should I watch for at home?”
- “What happens if my counts stay low for too long?”
There’s no shame in asking. The goal isn’t just to survive treatment. It’s to stay on it-without letting side effects derail your care.
Final Thought: It’s Manageable, But It’s Serious
Bone marrow suppression isn’t something you can ignore. It’s not a side effect you can just “tough out.” But it’s also not a death sentence. With smart monitoring, the right tools, and open communication with your care team, most people can get through it. The key is catching it early-and not letting fear stop you from speaking up.Low blood counts are a signal. Listen to them. Act on them. And don’t let the fear of side effects make you quit treatment before it has a chance to work.
Can bone marrow suppression be permanent?
In most cases, no. Once the medication is stopped or the dose adjusted, the bone marrow usually recovers within weeks. But in rare cases-especially with long-term use of certain drugs or in people with underlying bone marrow disorders-it can become chronic. If counts don’t improve after stopping the drug, a bone marrow biopsy may be needed to rule out other causes like myelodysplastic syndrome.
Can I take supplements to boost my blood counts?
No. Iron, folic acid, or vitamin B12 won’t fix bone marrow suppression caused by drugs. These supplements help with nutritional deficiencies, not drug-induced damage. In fact, taking iron without a confirmed deficiency can be harmful. Always check with your doctor before starting anything new.
Why do some people get severe suppression and others don’t?
It’s a mix of genetics, age, existing health, and drug metabolism. People over 65, those with kidney or liver disease, and those with certain gene mutations (like TP53) are at higher risk. Some people’s bodies break down drugs faster, reducing exposure. Others process them slowly, leading to buildup. That’s why personalized medicine is becoming the standard.
Is it safe to get vaccinated if I have low blood counts?
Inactivated vaccines (like flu, pneumonia, or COVID-19 shots) are generally safe, even with low counts. Live vaccines (like MMR or shingles) are not recommended during active suppression because your immune system can’t handle them safely. Always ask your oncologist before getting any shot.
Can I still work or go out in public?
It depends on your counts. If your neutrophil count is above 1,000, light activity is usually fine. But if it’s below 500, avoid crowds, public transit, and places with poor air quality. Wear a mask in hospitals or stores during flu season. Many patients find remote work or staggered hours help them stay safe while staying active.
What’s the difference between neutropenia and leukopenia?
Leukopenia means low total white blood cells. Neutropenia means low specifically neutrophils-the most important type for fighting bacteria. Neutropenia is the real danger because it’s the main defense against infection. You can have mild leukopenia without much risk, but even mild neutropenia increases infection chances.
Do growth factors like Neulasta cause bone loss?
Yes, in some cases. A 2022 study in the Journal of Clinical Oncology found that long-term use of G-CSF drugs like filgrastim and pegfilgrastim increased the risk of osteoporosis by 12.3% in older patients. This is why doctors now weigh the benefits against risks, especially in elderly patients or those already at risk for fractures.
How long does it take for blood counts to recover after stopping the drug?
Recovery time varies. For mild suppression, counts often bounce back in 1 to 2 weeks. For severe cases, especially with chemotherapy, it can take 3 to 6 weeks. If suppression is caused by azathioprine or another immunosuppressant, switching drugs can speed recovery to 4 to 6 weeks. Persistent suppression beyond 8 weeks needs further investigation.