Imagine this: you just got a new prescription. The label says "Take once daily". But in your language, "daily" doesn’t mean once a day-it means "every day," and you take it twice. You don’t realize the mistake until you feel dizzy, nauseous, or worse. This isn’t rare. It happens every day to millions of people who don’t speak English fluently. And it’s not about not trying to understand. It’s about the system not giving them a fair shot.
Why Translation Isn’t Just Helpful-It’s Life-Saving
Medication errors kill over 250,000 people in the U.S. every year. About one in five of those mistakes happen because patients didn’t understand their instructions. For non-English speakers, the risk jumps 1.5 to 3 times higher. That’s not a coincidence. It’s a system failure.
The problem isn’t that people don’t ask. It’s that pharmacies rarely offer clear answers in their language. A 2021 survey found only 57% of community pharmacies provide translated prescription labels. That means over 40% of patients are left guessing. And guesswork with pills? That’s how accidents happen.
Studies show that when instructions are properly translated, medication errors drop by up to 62%. One study in California found that patients using translated labels understood their meds 95% of the time-compared to just 45% with standard English labels. That’s not a small difference. That’s the difference between healing and hospitalization.
What Makes a Translation Actually Work?
Not all translations are created equal. A simple Google Translate copy of a prescription label? It’s dangerous. A 2020 FDA report found that automated translations had a 38% error rate. That means nearly 4 out of 10 instructions were wrong or misleading.
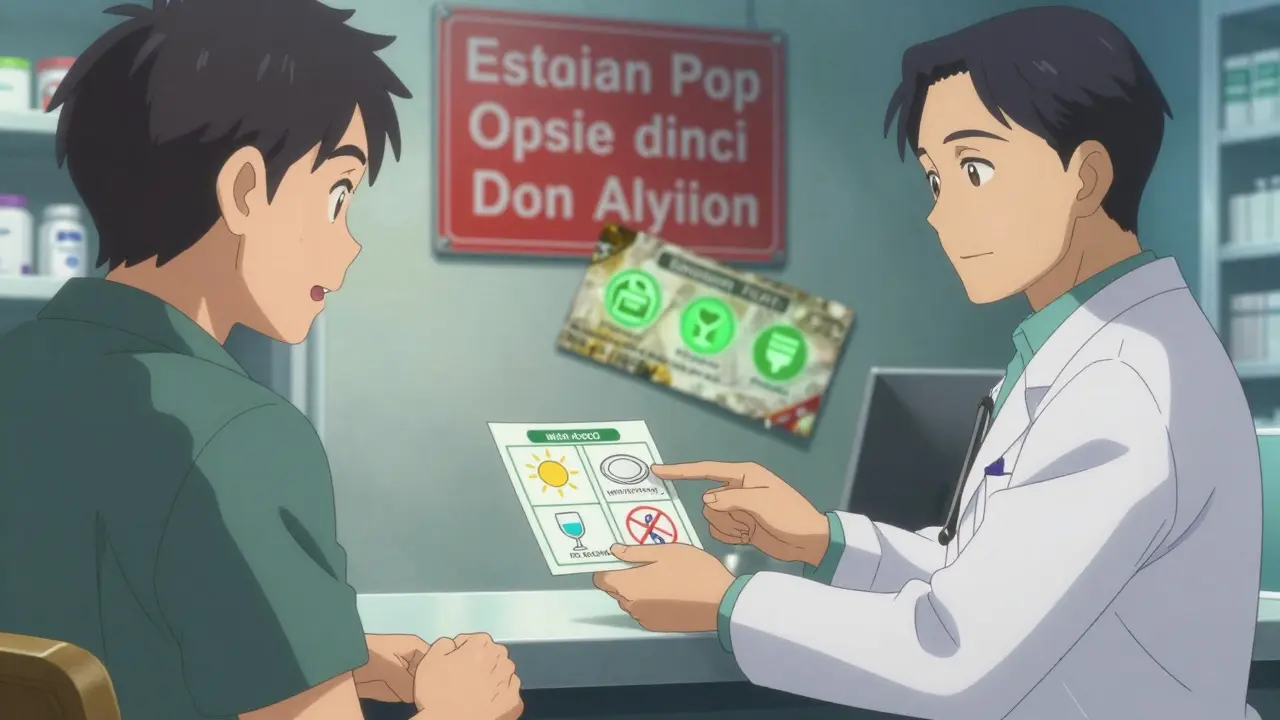
So what works? Three things:
- Plain language-No medical jargon. "Take one tablet by mouth every morning" instead of "Oral administration of one tablet QD."
- Universal symbols-Icons that mean "take with food," "avoid alcohol," or "shake well"-approved by ISO 3864 and FDA standards.
- Professional translation-Not just bilingual staff, but trained medical translators who understand drug names, dosages, and side effects in both languages.
The ConcordantRx project tested this. They rewrote prescription labels in Chinese, Korean, and Russian using plain language and pictograms. When tested, 100% of patients understood their instructions. Not 85%. Not 90%. 100%.
Compare that to pharmacies that rely on staff who speak a little Spanish or Vietnamese. A 2017 study found those efforts only led to 42% comprehension. Why? Because knowing a few phrases doesn’t mean knowing how to explain why a blood thinner should never be taken with grapefruit juice.
How Patients Are Really Feeling
Real stories tell the truth better than statistics.
A Korean woman in New York took her blood thinner twice a day because the label said "daily"-and she thought that meant "every day," not "once a day." She ended up in the ER with internal bleeding.
A Vietnamese man in California mixed his diabetes pills with his insulin because the label didn’t say which was which. He didn’t know the difference between "glimepiride" and "insulin glargine." The pharmacy didn’t help.
On Reddit, pharmacists admit they’re stuck. One wrote: "I had a patient who drank albuterol solution thinking it was a cough syrup. The label said "nebulizer solution." She didn’t know what a nebulizer was. We had no translator on call. I felt sick."
Healthgrades reviews show 63% of non-English speakers report confusion about their meds. The top complaints? "They didn’t check if I understood" and "No instructions in my language."
What Pharmacies Should Be Doing
It’s not rocket science. The U.S. Department of Health and Human Services laid out a clear plan called the LEP Toolkit. It has four parts:
- Ask-At check-in, ask: "What language do you prefer?" Don’t assume. Don’t skip it.
- Translate-Vital documents: prescription labels, warning stickers, side effect sheets. All in the patient’s language.
- Interpret-Use certified medical interpreters. Not family members. Not the cashier. A trained professional who knows medical terms.
- Follow up-Ask: "Can you tell me how to take this?" If they can’t, you haven’t done your job.
Pharmacies that do this see results: 58% fewer errors, 37% better adherence. That’s not just safer-it’s cheaper. Medication errors cost hospitals $5 billion a year. Investing in translation saves money.
The Technology That’s Making This Possible
Companies like RxTran, TransPerfect Healthcare, and LanguageLine are building systems that plug into pharmacy software like Rx30 and PioneerRx. They offer translations in 25+ languages-from Arabic to Tagalog to Somali.
Here’s what’s changing:
- Labels now include pictograms that show how to take the pill, what to avoid, and when to call the doctor.
- Pharmacies can print bilingual labels on the spot using integrated printers.
- Some systems now use QR codes. Scan it, and you hear the instructions spoken in your language.
But not all tech is good. AI translation tools are being pushed hard-but they’re risky. The FDA warned in 2023 that unvalidated AI translations had a 43% error rate. That’s worse than using a family member. Machines don’t know that "twice daily" in Chinese can mean "in the morning and at night"-or that "take with meals" might mean "with rice," not "with bread."

What’s Changing in 2026
California made it law: starting January 1, 2024, every pharmacy serving LEP patients must be certified. That means they must prove they have trained staff, translated materials, and a system to ask for language preferences.
New York City requires translation for the top 10 languages spoken in the city. Federal law still says Title VI of the Civil Rights Act requires "meaningful access"-but enforcement is weak.
Big changes are coming. By 2026, electronic health records will automatically flag a patient’s language preference and trigger translation services. Medicare plans now have to report how well they serve non-English speakers. And a new national standard-the CLAS in Pharmacy-is expected to be finalized in late 2024.
Pharmacies that act now will lead. Those that wait? They’ll be out of compliance-and out of trust.
What You Can Do
If you’re a patient:
- Always say your preferred language when picking up a prescription.
- Ask: "Can I get this label in my language?"
- Don’t let family members explain your meds. Ask for a professional interpreter.
- If you don’t understand, say so. Again. And again.
If you work in a pharmacy:
- Train your staff. Even 8 hours of cultural competency training changes outcomes.
- Use certified translation services-not Google Translate.
- Print bilingual labels. Use pictograms. Make it visual.
- Track your results. How many patients say they understand? Adjust.
Medication safety isn’t about fancy tech. It’s about basic human respect. If you hand someone a pill, you owe them a way to understand it. Not in English. In their language.
Why can’t pharmacies just use family members to translate?
Using family members sounds practical, but it’s risky. A 2022 report from the Institute for Safe Medication Practices found it leads to 65% more medication errors. Why? Family members may not know medical terms, may skip scary side effects to avoid worry, or may misremember doses. Worse, they might feel pressured to say "yes" even if they don’t understand. Certified interpreters are trained to translate accurately, maintain confidentiality, and ask follow-up questions. That’s why professional interpretation is the gold standard.
Are translated labels legally required?
Yes-at the federal level under Title VI of the Civil Rights Act, which says healthcare providers must offer meaningful access to non-English speakers. But enforcement varies. Some states like California and New York City have stricter rules, requiring pharmacies to provide translations for the top languages spoken in their area. Still, many pharmacies don’t comply. That’s why patient advocacy matters: if you ask for a translated label and get refused, you’re not being unreasonable-you’re exercising your rights.
What languages are most commonly needed for medication labels?
Based on U.S. population data and pharmacy surveys, the top five languages are Spanish, Chinese (both Simplified and Traditional), Vietnamese, Korean, and Russian. But demand is growing fast for languages like Arabic, Somali, Hmong, and Tagalog. Pharmacies serving diverse communities need to be ready for more than just the usual suspects. A 2023 study showed that patients speaking less common languages like Hmong had 82% higher misunderstanding rates because translations weren’t available at all.
How much does professional translation cost?
Professional translation services cost between $2.50 and $5.00 per prescription, depending on the language and complexity. That sounds expensive-but compare it to the cost of an ER visit from a medication error: $5,000 to $15,000. Pharmacies that invest in translation see lower error rates, fewer complaints, and higher patient loyalty. In fact, one University of Florida study found pharmacies with full language access had 22% higher patient satisfaction scores. The ROI isn’t just ethical-it’s financial.
What should I look for on a translated prescription label?
A good translated label has four things: 1) Clear instructions in plain language (no medical jargon), 2) Symbols that show how to take the medicine (like a sun for "take in morning" or a wine glass with a slash for "no alcohol"), 3) The drug name and dosage in both English and your language, and 4) A phone number to call if you have questions. If it’s just a word-for-word translation of an English label, it’s probably not helpful. Real translation means rethinking how the message is delivered-not just swapping words.