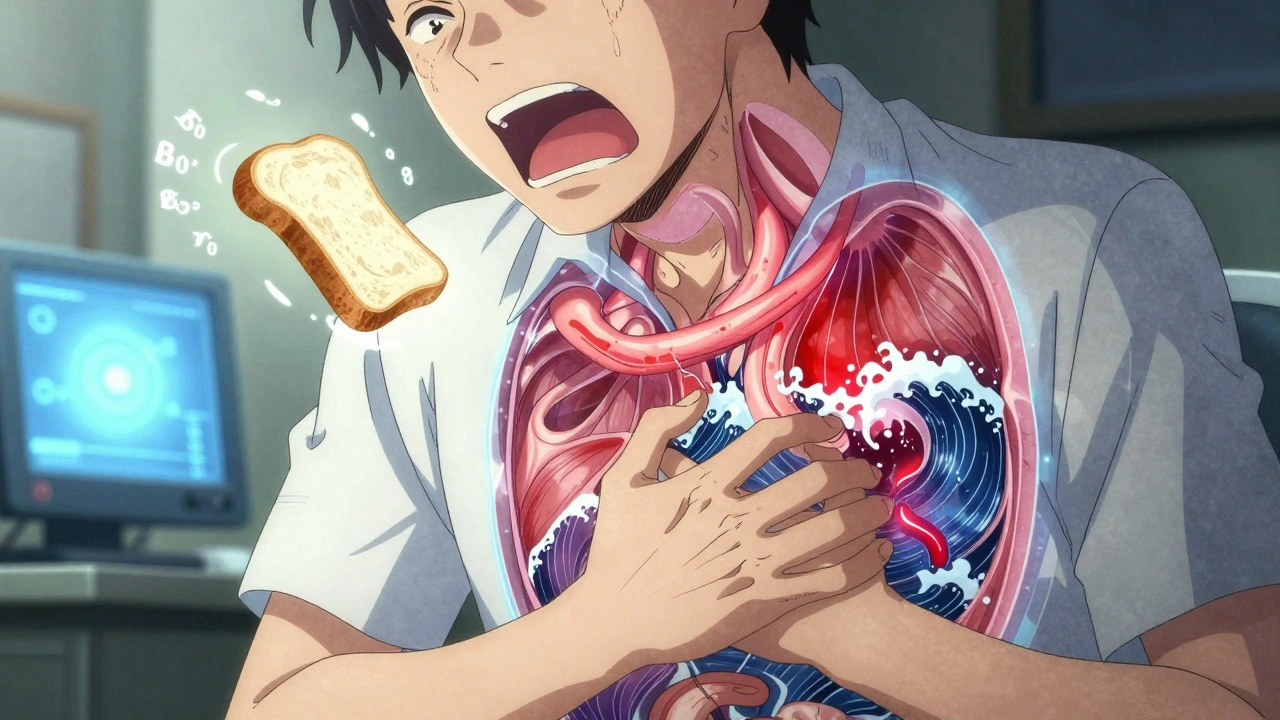
Swallowing feels automatic-until it doesn’t. If you’ve ever felt food get stuck, had chest pain after eating, or found yourself avoiding solid foods because it’s just too hard, you’re not alone. These aren’t just minor inconveniences. They’re signs of something deeper: esophageal motility disorders. These conditions mess with the coordinated muscle contractions that move food from your throat to your stomach. When those contractions fail, dysphagia follows. And the key to figuring out what’s really going on? High-resolution manometry.
What Exactly Is Going On in Your Esophagus?
Your esophagus isn’t just a passive tube. It’s a muscular pipeline that works like a wave. When you swallow, a perfect sequence of contractions-called peristalsis-pushes food down. At the bottom, the lower esophageal sphincter (LES) opens just enough to let food in, then snaps shut to keep stomach acid out. In esophageal motility disorders, this system breaks down. The muscles don’t contract in the right order, they contract too hard, or the LES won’t relax at all.There are two main types: primary and secondary. Primary disorders start in the esophagus itself. The most well-known is achalasia, where the LES stays tightly closed and the esophagus loses its ability to push food down. Then there’s jackhammer esophagus, where contractions are violent and prolonged, with pressures over 5,000 mmHg•s•cm. Nutcracker esophagus involves strong but coordinated contractions that still cause pain. Diffuse esophageal spasm throws random, uncoordinated contractions into the mix.
Secondary disorders come from elsewhere. Scleroderma, for example, affects up to 80% of people with the disease. The immune system attacks connective tissue, slowly stiffening the esophagus until it can’t move food properly. Diabetes, Parkinson’s, and even chronic acid reflux can also interfere with motility over time.
Dysphagia Isn’t Just ‘Hard to Swallow’
People often assume dysphagia means choking on food. But it’s more nuanced. In achalasia, patients usually start with trouble swallowing solids-bread, meat, rice-then later can’t handle liquids either. That’s because the esophagus loses its ability to generate any useful pressure. In spastic disorders like jackhammer esophagus, swallowing can trigger sharp, crushing chest pain that mimics a heart attack. Many end up in the ER multiple times before anyone checks their esophagus.Regurgitation is another big red flag. Not the occasional burp-this is undigested food coming back up hours after eating. Weight loss is common too. One study found 65% of achalasia patients lost 15 to 20 pounds before diagnosis. And it’s not just physical. A survey of over 1,200 people with these disorders showed 68% waited 2 to 5 years for a correct diagnosis. Forty-two percent saw three or more doctors. Too often, doctors treat it as GERD. Proton pump inhibitors (PPIs) are prescribed, but they do nothing if the problem isn’t acid-it’s muscle failure.
Why Manometry Is the Gold Standard
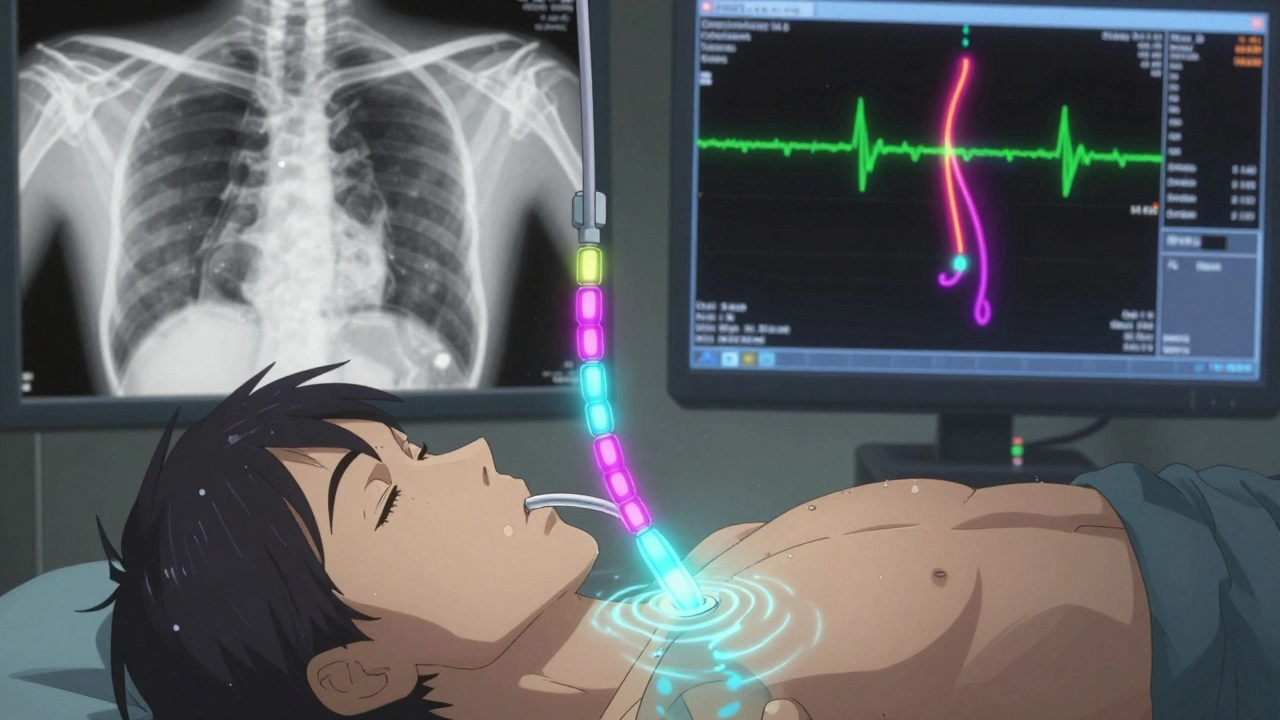
Endoscopy can rule out tumors or strictures, but it can’t see how the muscles are working. That’s where high-resolution manometry (HRM) comes in. A thin, flexible tube with 36 pressure sensors spaced 1 cm apart is passed through the nose into the esophagus. As you swallow water, the sensors record pressure changes across the entire length. The result? A color-coded map showing exactly where the contractions are weak, too strong, or missing.This isn’t just fancy tech-it changed everything. Before HRM, doctors relied on older methods like barium swallows, which showed structure but not function. HRM detects achalasia with 96% accuracy, compared to just 78% for barium. And it doesn’t stop there. The Chicago Classification v4.0, published in 2023, gives doctors a clear, standardized way to interpret those color maps. It defines what counts as a true disorder versus a normal variation. For example, it distinguishes between Type I, II, and III achalasia based on pressure patterns, which directly affects treatment choice.
Another key test is the Multiple Rapid Swallows (MRS). You swallow five quick sips in a row. In a healthy esophagus, the muscles reset after each swallow. In achalasia, they don’t. The distal contractile integral drops below 100 mmHg•s•cm. That’s a telltale sign of poor esophageal reserve.
What Are the Treatment Options?
Treatment depends on the diagnosis. For achalasia, the goal is to open the LES. Laparoscopic Heller myotomy (LHM) cuts the muscle fibers around the sphincter. It’s been around for decades and still works in 85-90% of cases after five years. But it can cause reflux. That’s why surgeons often add a partial fundoplication-a wrap of stomach tissue to prevent acid from backing up.Peroral endoscopic myotomy (POEM) is newer. Instead of cutting through the abdomen, the surgeon goes through the mouth with an endoscope. It’s less invasive, recovery is faster, and success rates match LHM. But POEM has a downside: 44% of patients develop reflux esophagitis within two years, compared to 29% with LHM.
Pneumatic dilation uses a balloon to stretch the LES. It’s cheaper and doesn’t require surgery, but it’s not permanent. About 25-35% of people need another dilation within five years. It’s often used for older patients or those who can’t tolerate surgery.
For jackhammer or nutcracker esophagus, medications like calcium channel blockers or nitrates can help relax the muscles. Botulinum toxin injections into the LES are another option, but the effect fades after 6-12 months. In severe cases, POEM can also be used to cut the overactive muscle bands.
Newer tools like the LINX device-a ring of magnetic beads placed around the LES-are being tested for select patients with preserved peristalsis. Early results show 75% symptom improvement at one year. And then there’s the SmartPill, a wireless capsule you swallow that records pressure and pH over 24-48 hours. It’s not as detailed as HRM, but it’s great for people who can’t tolerate tubes or need ambulatory monitoring.

Challenges and Real-World Gaps
HRM machines cost between $50,000 and $75,000. Training to interpret them takes months of specialized fellowship work. That’s why they’re mostly in academic hospitals and big cities. In rural areas or low-income countries, access is rare. Many patients never get tested. Even in the U.S., only 35% of community hospitals have HRM.Another issue? Overdiagnosis. Some pressure patterns look abnormal but don’t cause symptoms. Dr. C. Prakash Gyawali warns that labeling these as disorders can lead to unnecessary treatments. The Chicago Classification v4.0 tries to fix this by separating major disorders (which need treatment) from minor ones (which might not).
And then there’s the patient experience. One Reddit user wrote: “After my POEM, I ate a burger for the first time in seven years.” Another said: “I was on PPIs for eight years before they found jackhammer esophagus.” Misdiagnosis is still common. Proper education before the test helps-78% of patients report satisfaction when they understand what’s happening. That number drops to 45% if they’re just told to “swallow some water.”
What’s Next?
The field is moving fast. AI tools are being trained to read manometry tracings. One 2023 study showed AI identified achalasia with 92% accuracy-better than untrained doctors. Wireless motility capsules are becoming more reliable. And researchers are exploring new drugs that target the nerves controlling the esophagus.But the biggest shift is cultural. Doctors are starting to take dysphagia seriously-not as a side effect of aging or GERD, but as a sign of a real, treatable problem. The number of motility tests in the U.S. has grown 18% annually since 2018. That’s progress.
If you’ve struggled with swallowing for months-or years-and no one has looked beyond your stomach acid, ask for manometry. It’s not perfect. It’s not fun. But it’s the only way to know what’s really happening inside your esophagus. And knowing that can change everything.