Sickle Cell Kidney Function Calculator
This calculator estimates your kidney function using the MDRD equation. The results help you and your healthcare provider monitor kidney health in sickle cell anemia.
Kidney Function Results
What do these results mean?
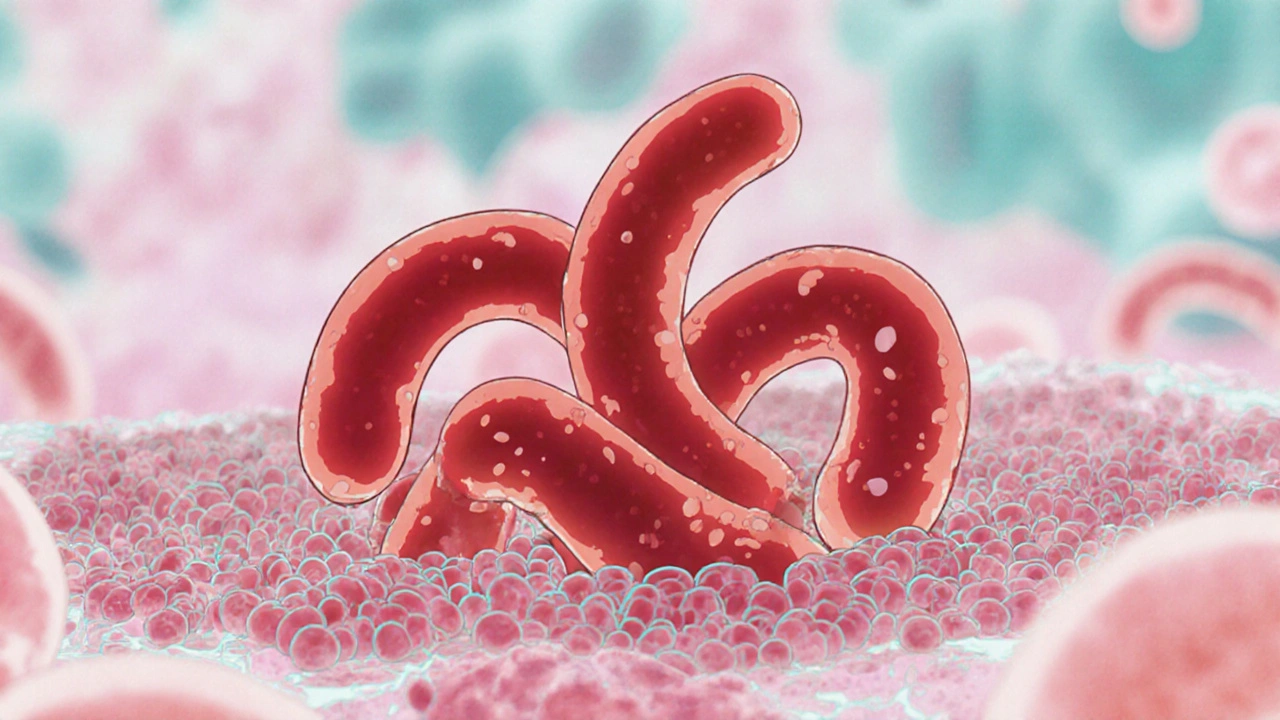
Imagine living with a condition that turns your red blood cells into tiny, rigid crescents that can jam up tiny blood vessels. Now add the threat of those blockages hurting the organs that keep your body clean and balanced. That’s the reality for many people with Sickle Cell Anemia a genetic blood disorder caused by a mutation in the beta‑globin gene, producing abnormal hemoglobin S. The kidneys, which filter thousands of liters of blood every day, are especially vulnerable. This article unpacks why sickle cell anemia and kidney disease often walk hand‑in‑hand and shows you how to spot, test, and manage the connection.
What Is Sickle Cell Anemia?
Sickle cell anemia (SCA) stems from a single‑letter change in the gene that makes hemoglobin, the protein that carries oxygen. The altered protein, called hemoglobin S, sticks together when oxygen drops, forcing red cells into a sickle shape. These misshapen cells are less flexible, break down faster, and can block capillaries. Over time, the repeated blockages-known as vaso‑occlusive crises-damage tissues throughout the body, from the bones to the brain.
Why the Kidneys Are at Risk
The kidneys receive about 20% of the heart’s output, which means millions of sickled cells pass through their tiny filtering units called glomeruli every minute. When a sickle cell slips into a glomerular capillary, it can cause:
- Ischemia (lack of oxygen) that injures the delicate filtration membrane.
- Inflammation that thickens the basement membrane.
- Obstruction that raises pressure inside the tiny vessels, eventually scarring them.
These processes, collectively dubbed Sickle Cell Nephropathy a spectrum of kidney damage ranging from mild protein leakage to complete renal failure, set the stage for chronic kidney disease (CKD).
Common Kidney Problems Linked to Sickle Cell
People with SCA can develop several distinct kidney issues, each with its own warning signs:
- Hyposthenuria: The kidneys lose the ability to concentrate urine, leading to frequent, dilute urination.
- Proteinuria: Small amounts of protein spill into the urine, an early red flag for glomerular damage.
- Glomerulopathy: Scarring of the glomeruli that gradually reduces filtration capacity.
- Chronic Kidney Disease (CKD): Defined by a sustained drop in glomerular filtration rate (GFR) below 60 ml/min/1.73 m² for three months or more.
- End‑Stage Renal Disease (ESRD): When GFR falls under 15 ml/min/1.73 m², dialysis or transplantation becomes necessary.
According to a 2023 multicenter study, roughly 30% of adults with sickle cell develop proteinuria by age 40, and about 12% progress to ESRD before age 50.

Risk Factors and Early Warning Signs
Not everyone with SCA will face severe kidney disease, but certain factors heighten the risk:
- Repeated severe vaso‑occlusive crises, especially those involving the abdomen.
- High blood pressure (hypertension) that adds extra strain on already compromised glomeruli.
- Chronic anemia that forces the kidneys to work harder to deliver oxygen.
- Use of nephrotoxic medications, such as non‑steroidal anti‑inflammatory drugs (NSAIDs).
Early signs you should never ignore:
- Persistent swelling in the ankles or around the eyes.
- Dark‑colored or foamy urine.
- Unexplained fatigue that doesn’t improve with transfusion.
- Elevated blood pressure measured on two separate visits.
How Doctors Diagnose Kidney Involvement
Screening begins with simple, non‑invasive tests:
- Urine dipstick for protein and blood.
- Serum creatinine and calculated eGFR to gauge filtration.
- Blood pressure monitoring at every routine visit.
If abnormalities appear, the next step is a more detailed work‑up. A Renal Ultrasound imaging that assesses kidney size, cortical thickness, and blood flow can rule out structural issues. In some cases, a kidney biopsy is performed to confirm glomerulopathy and guide therapy.
Managing Kidney Health in Sickle Cell
There’s no single cure for sickle‑related kidney disease, but a combination of therapies can slow progression:
- Hydroxyurea: Increases fetal hemoglobin (HbF), reducing sickling episodes and, in several trials, lowering proteinuria rates.
- Regular blood transfusions: Dilutes sickle cells, improving oxygen delivery and protecting the kidneys.
- ACE inhibitors or ARBs: Lower intraglomerular pressure and cut protein loss.
- Blood pressure control: Target < 130/80 mmHg, using lifestyle changes and medication as needed.
- Avoid nephrotoxins: Swap NSAIDs for acetaminophen and discuss any new drugs with a nephrologist.
Nutrition also matters. A low‑salt, moderate‑protein diet eases the kidneys’ workload, while staying well‑hydrated helps keep sickle cells from clumping.

Living with Both Conditions: Practical Tips
Daily habits can make a huge difference:
- Track blood pressure at home and keep a log for your doctor.
- Schedule kidney labs at least twice a year, even if you feel fine.
- Stay on a steady medication schedule; missed hydroxyurea doses can trigger crises.
- Carry a medical alert card that lists both sickle cell and kidney disease.
- Join a support group-shared experiences often reveal tricks that aren’t in textbooks.
Remember, early detection is the best defense. When proteinuria is caught early, ACE inhibitors can often bring urine protein back to normal levels.
Quick Reference Table
| Age Group | % with Proteinuria | % with CKD (GFR <60) | % with ESRD |
|---|---|---|---|
| 0‑12 years | 5 | 1 | <1 |
| 13‑25 years | 18 | 7 | 2 |
| 26‑40 years | 32 | 15 | 6 |
| 41+ years | 45 | 28 | 12 |
Frequently Asked Questions
Can sickle cell patients live a normal life without kidney problems?
Many individuals with sickle cell never develop severe kidney disease, especially if they receive regular monitoring and early treatment. However, because the kidneys are constantly exposed to sickled cells, a lifelong surveillance plan is recommended.
What is the best test to catch early kidney damage?
A urine protein‑to‑creatinine ratio (UPCR) combined with an estimated glomerular filtration rate (eGFR) provides the most sensitive early detection. Annual testing becomes crucial after puberty.
Does hydroxyurea really protect the kidneys?
Clinical trials from 2020‑2023 show that patients on hydroxyurea have a 30% lower incidence of new‑onset proteinuria compared to those not taking it. The drug’s ability to raise fetal hemoglobin reduces sickling episodes that damage renal tissue.
Are there dietary changes that help?
A diet low in sodium (<2 g/day) and moderate in protein (0.8‑1 g/kg body weight) eases the kidneys’ workload. Staying well‑hydrated-about 2‑3 L of water daily-helps keep blood less viscous.
When should dialysis be considered?
Dialysis is advised when eGFR drops below 15 ml/min/1.73 m², when severe fluid overload, electrolyte imbalance, or uremic symptoms appear. Early referral to a nephrologist can help plan for pre‑emptive transplantation if eligible.