TNF Inhibitor TB Risk Calculator
Understand Your TB Risk
This calculator shows your TB reactivation risk based on the TNF inhibitor you're taking and your country of origin. It's based on the latest clinical guidelines and research.
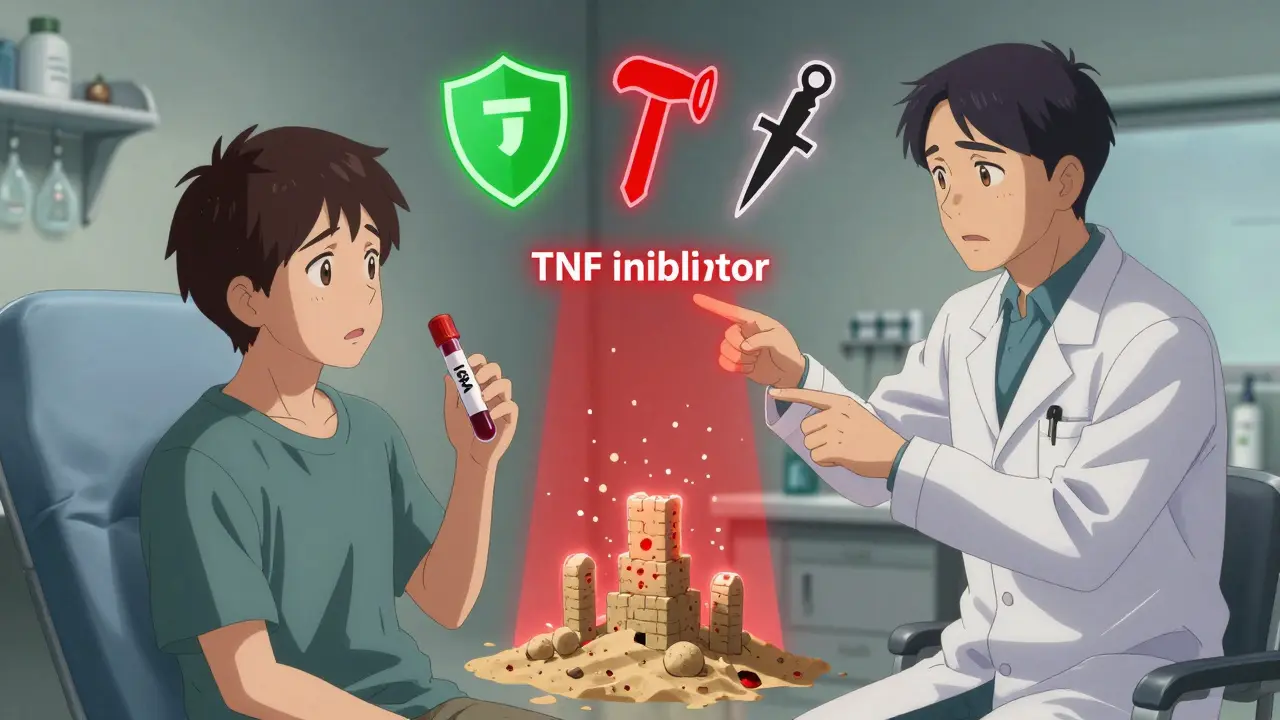
When you start a TNF inhibitor for rheumatoid arthritis, psoriasis, or Crohn’s disease, you’re getting powerful relief from inflammation. But behind that benefit is a quiet, serious risk: TB reactivation. It’s not common, but when it happens, it can be deadly. And the risk isn’t the same for every drug. Some TNF inhibitors are far more likely to wake up latent tuberculosis than others. Knowing which ones, why, and how to protect yourself isn’t optional-it’s life-saving.
Why TNF Inhibitors Can Reactivate TB
Your body keeps tuberculosis in check by building tiny walls of immune cells around the bacteria. These are called granulomas. They’re not perfect, but they work-most of the time. That’s why 1 in 4 people globally have latent TB: they’re infected, but not sick. Their immune system holds it at bay. TNF-alpha is the glue that holds those granulomas together. When you take a TNF inhibitor, you’re blocking that glue. Without it, the walls crumble. The bacteria wake up. And if you’re not screened, you might not know you’re at risk until you’re coughing blood or your spine is infected. Not all TNF inhibitors are the same. There are two main types:- Class 1: Etanercept-a soluble receptor that binds mainly to free-floating TNF-alpha. It leaves the membrane-bound version mostly untouched. That’s why it’s the safest option for TB risk.
- Class 2 and 3: Adalimumab and infliximab-antibodies that latch onto both free and membrane-bound TNF-alpha. This is the problem. They tear down the granuloma walls completely.
Screening Before You Start
Before you get your first shot or infusion, you need two things: a test and a conversation. The two standard tests are:- Tuberculin Skin Test (TST)-a bump on your arm after a shot. It’s cheap, widely available, but can give false positives if you’ve had the BCG vaccine (common outside the U.S.).
- Interferon-Gamma Release Assay (IGRA)-a blood test. More accurate for people with BCG exposure, but more expensive and not available everywhere.
What Happens If You Test Positive
If you have latent TB, you don’t need to stop your treatment plan-you just need to delay it by a few weeks. The goal is to kill the dormant bacteria before you suppress your immune system. Standard treatment is:- Isoniazid for 9 months-the old standard. Effective, but hard to stick with. About 32% of patients quit because of liver issues or just forgetting.
- Rifampin for 4 months-newer, better tolerated. FDA-approved in 2024. Adherence jumped from 68% to 89% in trials.
- Isoniazid + rifapentine once a week for 3 months-directly observed therapy helps, especially for people with unstable housing or substance use.

Monitoring After You Start
Screening isn’t a one-time thing. Most TB cases happen in the first six months after starting treatment. In fact, 78% of cases in one study were extrapulmonary-meaning TB showed up in the spine, kidneys, brain, or lymph nodes, not the lungs. That makes it harder to diagnose. Fever, night sweats, weight loss, fatigue-these are red flags. But they’re also common side effects of autoimmune disease flares. That’s why doctors need to think TB first, especially in the first year. Guidelines recommend:- Check for symptoms every three months for the first year, then annually.
- Don’t ignore a cough that won’t go away, even if it’s mild.
- Consider a chest X-ray if you have any symptoms-even if your TB test was negative.
Real-World Problems
In theory, this all sounds simple. In practice? It’s messy. A 2023 review of 1,200 patients found that 18% of TB cases happened in people who had negative screening results. Some of these patients had just moved to the U.S. from a high-risk country. Their infection was too new to show up on tests. Others had false negatives because their immune systems were already weakened by disease or steroids. And then there’s access. In rural clinics or low-income countries, IGRA isn’t available. TST is the only option. But if you’ve had the BCG vaccine, you’ll likely test positive-even if you don’t have TB. That leads to unnecessary treatment delays. One rheumatology nurse on Reddit said she once held off starting adalimumab for six months because of a positive TST in a patient from Vietnam-only to find out later the patient had never had the BCG shot. Also, 27% of patients in a 2022 ACR survey had their TNF inhibitor treatment delayed because their LTBI treatment wasn’t properly documented. A simple note in the chart can mean the difference between starting on time and waiting months.
What’s Changing in 2025
The field is moving toward smarter solutions. New drugs are being tested that block TNF-alpha without touching the membrane-bound version. Early animal studies show an 80% drop in TB reactivation. These selective inhibitors could be the next generation of biologics. In the meantime, the safest approach is still:- Screen everyone before starting.
- Treat latent TB before biologics-especially if you’re from a high-burden country.
- Use rifampin or the 3-month combo if possible to improve adherence.
- Monitor for symptoms every three months for the first year.
- Don’t assume a negative test means you’re safe.
Bottom Line
TNF inhibitors change lives. But they don’t come with a safety net. The risk of TB reactivation is real, predictable, and preventable. The difference between getting sick and staying well often comes down to one simple step: asking, “Have I been tested for TB?” Don’t wait for symptoms. Don’t assume your doctor will bring it up. Be the one who asks. Be the one who follows through. Because when it comes to your immune system and TB, there’s no room for guesswork.Can you get TB even if your screening test is negative?
Yes. Up to 18% of TB cases in TNF inhibitor users occur in people with negative screening results. This can happen if the infection is very recent, the immune system is too weak to react to the test, or the test has low sensitivity in certain populations. That’s why ongoing symptom monitoring is just as important as the initial test.
Which TNF inhibitor has the lowest TB risk?
Etanercept has the lowest risk. Studies show patients on etanercept are about 5 times less likely to develop TB than those on infliximab or adalimumab. This is because etanercept doesn’t bind to membrane-bound TNF-alpha, which is essential for keeping TB bacteria contained in granulomas.
Do I need to be treated for latent TB if I’m from a high-risk country?
Yes, even if your test is negative. Major guidelines, including EULAR 2023, recommend treating latent TB in people from countries with more than 40 TB cases per 100,000 people annually-regardless of test results. The risk of missing a latent infection in these populations is too high to rely on imperfect tests.
How long after starting a TNF inhibitor does TB usually appear?
Most cases occur within 3 to 6 months of starting therapy, especially with infliximab and adalimumab. But TB can develop anytime-even years later. The highest risk is in the first year, so symptom checks should be done every three months during that period.
Can I still take TNF inhibitors if I’ve had TB before?
Yes, but only after completing full treatment for active TB and waiting at least 3 months. You’ll need close monitoring, and your doctor may avoid the highest-risk drugs like infliximab. Some patients with prior TB develop TB-IRIS when starting biologics, so steroid coverage may be needed.
Is TB screening covered by insurance?
Yes, in the U.S., most insurance plans cover TST and IGRA when ordered before starting biologic therapy. Medicare and Medicaid require it. The cost is usually $150-$300, but it’s considered a mandatory pre-treatment step, not an optional test.
What if I can’t afford the 9-month isoniazid course?
Ask your doctor about the 4-month rifampin regimen or the 3-month weekly combo of isoniazid and rifapentine. These are newer, shorter, and have higher completion rates. Many public health clinics offer free or low-cost treatment through TB control programs.
Are biosimilar TNF inhibitors safer than brand-name ones?
No. Biosimilars of adalimumab and infliximab have the same biological structure and mechanism of action as the originals. They carry the same TB risk. The only difference is cost-they’re cheaper, but not safer.