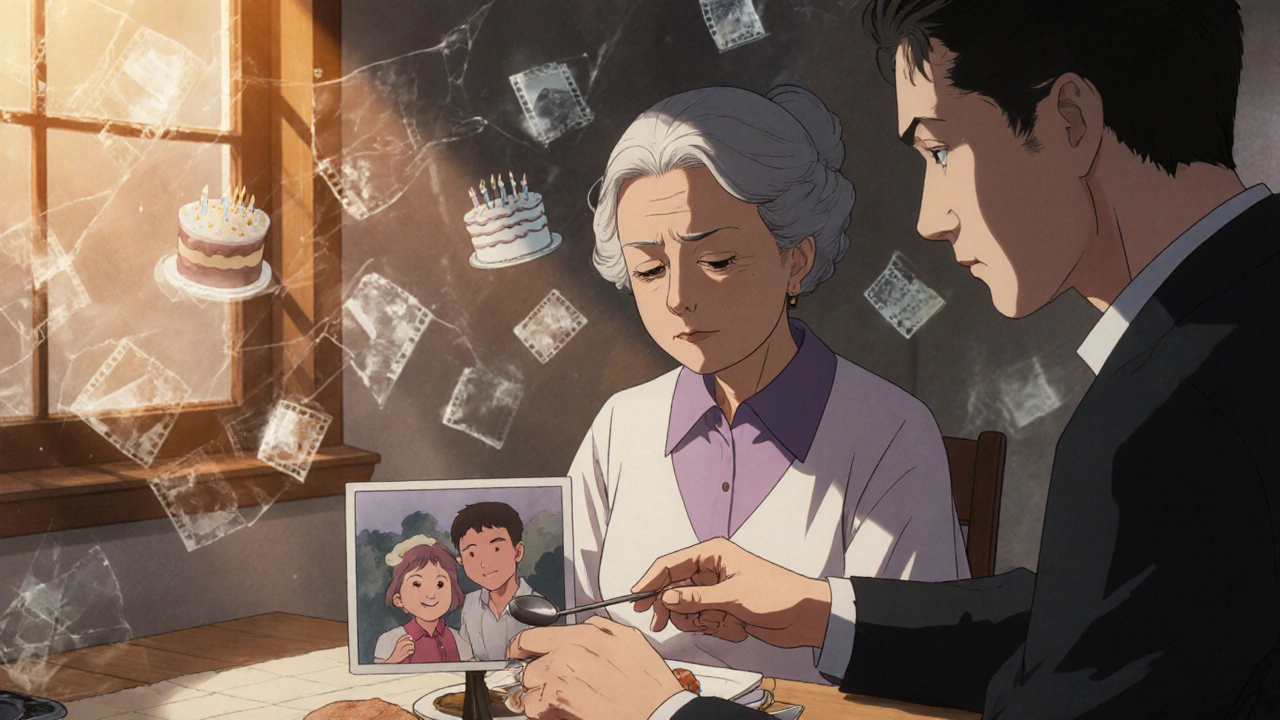
Alzheimer’s disease isn’t just forgetting where you put your keys. It’s losing the ability to recognize your own children, forgetting how to tie your shoes, or no longer remembering the name of the person you’ve lived with for 50 years. It’s the most common cause of dementia, affecting 60-80% of all dementia cases worldwide. By 2025, over 7 million Americans over 65 are living with it-and that number is climbing fast. If you or someone you love is facing this, you’re not alone. But understanding what’s happening inside the brain, how it unfolds over time, and what treatments actually work today can make all the difference.
What’s Really Happening in the Brain?
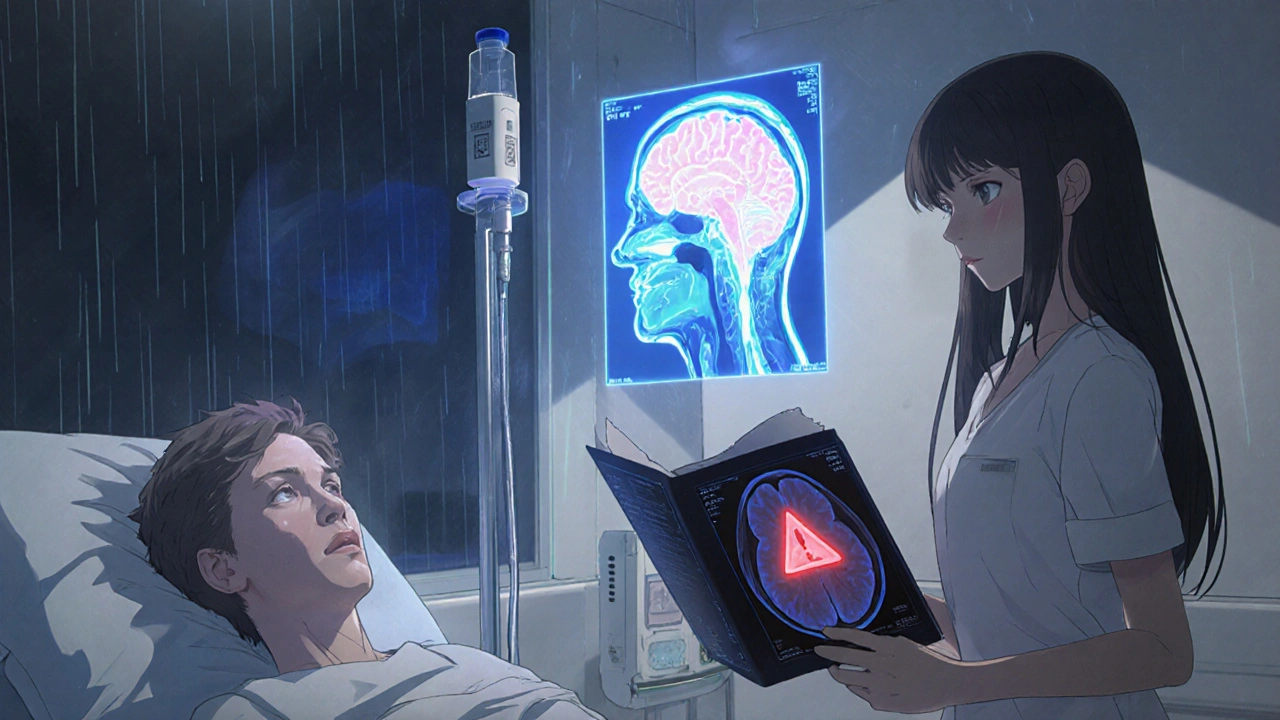
Alzheimer’s isn’t just aging. It’s a physical breakdown of brain cells. Two abnormal structures show up in the brains of people with Alzheimer’s: amyloid plaques and neurofibrillary tangles. Plaques are sticky clumps of a protein called beta-amyloid that build up between nerve cells. Tangles are twisted fibers of another protein, tau, that collapse inside the cells. These gunk up communication between neurons, starve them of nutrients, and eventually kill them.
The damage starts quietly, often in the hippocampus-the part of the brain that forms new memories. That’s why the earliest sign is usually trouble remembering recent events: what you ate for breakfast, a conversation from yesterday, or where you parked the car. As the disease spreads, it hits areas controlling language, reasoning, and judgment. By the time someone can’t recall their own birthday or gets lost in their own neighborhood, the brain has already lost massive amounts of tissue.
Doctors now use biomarkers to confirm Alzheimer’s before symptoms get severe. Cerebrospinal fluid tests can detect low levels of amyloid-beta and high levels of phosphorylated tau. Amyloid PET scans show plaque buildup with 92% accuracy. Tau PET scans are newer but still useful. These tools aren’t available everywhere-only 35% of U.S. clinics offer them-but they’re changing how we diagnose. No more guessing. If the biomarkers match, it’s Alzheimer’s.
The Seven Stages: How It Progresses
Alzheimer’s doesn’t hit all at once. It creeps in, then climbs. Experts break it into seven stages:
- Stage 1: No impairment-No symptoms. Brain changes may already be happening, but nothing shows up in daily life.
- Stage 2: Very mild decline-Minor memory lapses, like forgetting names. Often dismissed as normal aging.
- Stage 3: Mild decline-Friends or family start noticing. Trouble remembering words, losing things, forgetting appointments. This is often when people first seek help.
- Stage 4: Moderate decline-Clear memory loss. Forgetting recent events, struggling with finances, avoiding social situations. Diagnosis is common at this stage.
- Stage 5: Moderately severe decline-Needs help with daily tasks. Forgets major details like address or phone number. May not remember what year it is.
- Stage 6: Severe decline-Loses ability to recognize loved ones. Needs help dressing, bathing, using the toilet. May have hallucinations or become agitated.
- Stage 7: Very severe decline-Loses speech, can’t walk, swallows poorly. Fully dependent. This is the final stage.
On average, people live 4 to 8 years after diagnosis. Some live up to 20. It depends on age, overall health, and how well care is managed. The middle stage-where confusion grows and personality changes happen-is often the longest and most taxing for families.
Current Medications: What Works and What Doesn’t
There are no cures. But there are drugs that can help manage symptoms-and now, a few that might slow the disease itself.
Cholinesterase inhibitors-donepezil (Aricept), rivastigmine (Exelon), galantamine (Razadyne)-are the oldest. They boost a brain chemical called acetylcholine, which helps with memory and thinking. They work for about 40-50% of people, giving 3 to 6 months of stability. Side effects? Nausea, vomiting, diarrhea, sleep problems. Some people stop taking them because the downsides outweigh the benefits.
Memantine (Namenda) works differently. It blocks excess glutamate, a brain chemical that can damage neurons when overactive. It’s used for moderate to severe Alzheimer’s. It doesn’t improve memory, but it can slow the drop in function. Often combined with cholinesterase inhibitors.
These drugs don’t stop the disease. They just make the ride a little smoother-for a while.
The New Wave: Disease-Modifying Therapies
In January 2025, the FDA gave full approval to lecanemab (Leqembi), the first Alzheimer’s drug proven to slow decline-not just symptoms. In a trial of nearly 1,800 people, it reduced cognitive decline by 27% over 18 months. That’s not a cure. But for families watching a loved one fade, even a small delay matters.
Another drug, donanemab, showed even stronger results: 35% slowing of decline in its trial. Both are monoclonal antibodies given by IV infusion every two weeks. They work by clearing amyloid plaques from the brain.
But they come with serious risks. About 12.5% of people on lecanemab and 24% on donanemab develop ARIA-amyloid-related imaging abnormalities. That means brain swelling or tiny bleeds. It’s often symptom-free, but can be dangerous. That’s why patients need regular MRI scans-monthly at first. Many caregivers say the stress of constant monitoring is almost as heavy as the disease itself.
There’s also ALZ-801, an oral pill for people with two copies of the APOE-e4 gene (a major genetic risk factor). In trials, it cut cognitive decline by 81% in this group. It’s not approved yet, but if it is, it could be a game-changer for a specific subgroup.
Cost is another barrier. These drugs run about $26,500 a year. Medicare covers them, but only under strict rules. Many insurers still deny coverage. Only about 3% of eligible patients in the U.S. are getting them-not because they don’t work, but because the system isn’t ready.
Non-Drug Approaches That Actually Help
Medications aren’t the whole story. Some of the most powerful tools are lifestyle-based.
Cognitive stimulation therapy (CST) involves group activities-games, discussions, memory exercises. A 2024 review of 12 studies found it improved cognition enough to make a real difference in daily life. It’s simple. It’s cheap. And it works.
The FINGER study from Finland showed that a combo of healthy eating, regular exercise, brain training, and managing blood pressure and cholesterol cut cognitive decline by 25% over two years. People didn’t need drugs. They just changed how they lived.
Other proven supports include music therapy, art programs, and structured routines. For someone in the middle stage, a familiar song can spark memories. A daily schedule reduces confusion. A calm environment lowers agitation.
And caregivers? They need help too. The Alzheimer’s Association’s 24/7 helpline fielded over a million calls in 2024. Support groups, training programs, respite care-these aren’t luxuries. They’re lifelines.
The Big Picture: Where We Are Now
Alzheimer’s research is moving faster than ever. Blood tests are coming that can detect Alzheimer’s with 97% accuracy for under $500-down from $5,000 for PET scans. That means early detection could become routine, like a cholesterol test.
Scientists are now testing drugs that target tau proteins, inflammation, metabolism, and even gut health. Over 120 clinical trials are active, many combining therapies. The future isn’t one magic pill. It’s a personalized plan-based on your genes, your biomarkers, your lifestyle.
But gaps remain. Only 8% of trial participants are non-white, even though dementia affects Black and Hispanic populations at higher rates. Most treatment centers are in cities. Rural families get left behind. Caregivers-mostly women-lose jobs, savings, and mental health. One in three seniors dies with Alzheimer’s or another dementia. It’s the sixth leading cause of death in the U.S.
And yet, there’s hope. We can now detect it early. We have drugs that slow it. We know lifestyle changes matter. We’re learning how to support families better. The tools are here. What’s missing is access, equity, and urgency.
What You Can Do Right Now
If you’re worried about memory loss:
- See a doctor-don’t wait. Early diagnosis opens more options.
- Ask about biomarker testing. Even if you can’t get a PET scan, blood tests are becoming available.
- Start living healthier: walk daily, eat vegetables and fish, manage blood pressure, get hearing checked.
- If you’re a caregiver: join a support group. You’re not alone. Ask for help. Take breaks.
- Use resources like the Alzheimer’s Association (1.800.272.3900). They offer free guides, webinars, and counseling.
This disease doesn’t just steal memories. It steals time, independence, and peace. But with the right knowledge and support, you can fight back-not with magic, but with science, strategy, and care.
Can Alzheimer’s be cured?
No, there is no cure yet. But new treatments like lecanemab and donanemab can slow the progression of symptoms in early-stage patients. These drugs don’t reverse damage, but they can delay decline by months to over a year, giving families more time with their loved ones.
Are memory lapses always a sign of Alzheimer’s?
Not at all. Forgetting where you put your keys or blanking on a name is normal aging. Alzheimer’s involves consistent, worsening memory loss that interferes with daily life-like forgetting how to get home, not recognizing family members, or being unable to manage bills. If memory problems are getting worse and affecting routines, it’s time to see a doctor.
How do I know if a new treatment is right for my loved one?
Start with a specialist-a neurologist or geriatrician. They’ll check for biomarkers, genetic risk (like APOE-e4), and overall health. New drugs like lecanemab are only for early-stage patients with confirmed amyloid plaques. They’re not for late-stage or people with other serious conditions. The risks (like brain swelling) need to be weighed against potential benefits. Ask about insurance coverage and nearby infusion centers.
Why are some Alzheimer’s drugs so expensive?
These are biologic drugs made with complex processes, requiring specialized manufacturing and monitoring. The cost also includes the infrastructure: monthly MRIs, infusion centers, and specialist oversight. Medicare covers them, but many private insurers still resist. The $26,500 annual price tag reflects R&D costs, but critics argue the clinical benefit doesn’t justify the cost for many patients.
Can Alzheimer’s be prevented?
There’s no guaranteed prevention, but up to 40% of dementia cases may be delayed or prevented by managing risk factors. Control blood pressure, avoid obesity, treat hearing loss, stay physically active, eat a Mediterranean-style diet, and keep your brain engaged. These steps aren’t just good for the brain-they’re good for the heart, too.
What should I do if my parent refuses to see a doctor?
Start with a general check-up for something else-like high blood pressure or a routine physical. Bring up memory concerns gently: "I’ve noticed you’ve been forgetting things lately. Maybe the doctor can check your brain health too?" Many people fear the diagnosis and avoid it. Frame it as staying healthy, not as admitting something’s wrong. You can also call the Alzheimer’s Association helpline for advice on how to approach the conversation.

