Hyperkalemia Medication Risk Checker
Medication Risk Assessment
Check if your medication combinations could put you at risk for dangerous hyperkalemia. This tool is based on guidelines from the article "Dangerous Hyperkalemia from Medications: Cardiac Risks and Treatment".
Important: This tool is for informational purposes only. Always consult with your healthcare provider for personalized medical advice.
What Is Hyperkalemia-and Why Should You Care?
Hyperkalemia means your blood potassium level is too high. It’s not just a lab number-it’s a silent threat to your heart. When potassium climbs above 5.5 mEq/L, your heart’s rhythm can start to wobble. At 6.5 mEq/L or higher, you’re in danger of sudden cardiac arrest. And here’s the twist: you might not feel a thing until it’s too late.
This isn’t rare. About 2-3% of the general population has it. But if you’re on blood pressure or heart failure meds like lisinopril, losartan, or spironolactone? Your risk jumps to 10-20%. That’s one in five people. And many of them are told to keep taking those meds because they’re life-saving. So what do you do?
Which Medications Cause High Potassium?
It’s not one drug. It’s combinations. The biggest culprits are medications that protect your heart and kidneys-but also block potassium from leaving your body.
- ACE inhibitors (like lisinopril)
- ARBs (like losartan)
- Mineralocorticoid receptor antagonists (like spironolactone and eplerenone)
- Potassium-sparing diuretics (like amiloride and triamterene)
- Direct renin inhibitors (like aliskiren)
Here’s the scary part: using spironolactone with an ACE inhibitor or ARB, plus a common antibiotic like co-trimoxazole, can make sudden death 5.5 times more likely than using spironolactone alone. That’s not a small risk. That’s a red flag.
People with kidney disease, diabetes, or over 65 are at higher risk. Dehydration makes it worse. Even skipping a few days of water can push potassium into danger zones.
How High Potassium Attacks Your Heart
Your heart works because of tiny electrical signals. Potassium helps control those signals. Too much potassium messes with the electrical rhythm. At first, you might see nothing on an ECG. But as levels rise, the signs appear like warning lights:
- 5.5-6.5 mEq/L: Tall, pointy T-waves-your heart’s first cry for help.
- 6.5-7.5 mEq/L: PR interval stretches out. The signal slows down.
- Over 7.5 mEq/L: QRS complex widens. Your heart’s electrical system is breaking down.
- Over 8 mEq/L: Sine wave pattern. Then-ventricular fibrillation. No pulse. No time.
This isn’t theoretical. A 2024 study in the Journal of the American Heart Association showed patients with hyperkalemia had far more heart attacks, strokes, and dangerous arrhythmias than those with normal potassium-even when they were on the same heart meds.
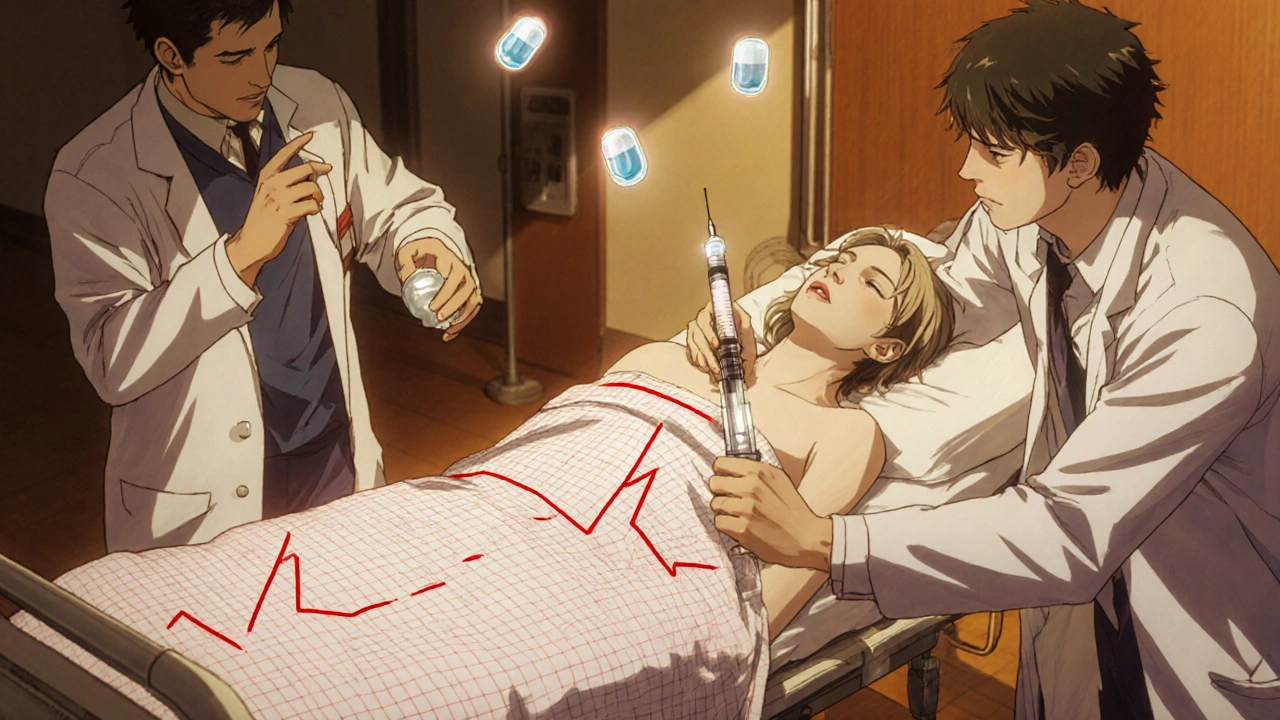
Emergency Treatment: What Happens in the Hospital
If your potassium hits 6.5 mEq/L or higher-and especially if your ECG is changing-you need immediate treatment. No waiting. No delays.
- Calcium gluconate (1-2 grams IV): This doesn’t lower potassium. It protects your heart. Within minutes, it stabilizes the heart muscle and reverses dangerous ECG changes. It’s the first line of defense.
- Insulin and glucose (10 units insulin + 25g glucose IV): This pushes potassium into your cells. Levels drop by 0.5-1.5 mEq/L within 15-30 minutes.
- Albuterol nebulizer (50-100 mcg): Another way to shift potassium into cells. Lowers levels by 0.5-1.0 mEq/L. Works fast.
- Dialysis: If you have kidney failure, this is the only way to remove potassium fast enough.
These steps buy you time. But they don’t fix the root problem. That’s where long-term management comes in.
Keeping Potassium in Check Long-Term
For many people, stopping their heart or kidney meds isn’t an option. Those drugs reduce death risk by 20-30%. So what’s the solution?
Two new drugs changed the game: patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma). These aren’t diuretics. They’re potassium binders. You take them by mouth. They trap potassium in your gut and flush it out in your stool.
Studies show they lower potassium by 0.4-1.0 mEq/L within hours. And they let people stay on their life-saving meds. One trial found 86% of patients stayed on their RAASi dose with patiromer-compared to only 66% without it.
Side effects? Constipation in 15-20%. Diarrhea in 10-15%. But compared to the risk of a heart attack? Most patients and doctors agree it’s worth it.

What You Can Do at Home
If you’re on any of these meds, here’s what you need to do:
- Get your potassium checked every 1-4 weeks, especially when starting or changing meds.
- Avoid salt substitutes. Many contain potassium chloride. One teaspoon can add 1,000 mg of potassium.
- Limit high-potassium foods: Bananas, oranges, potatoes, tomatoes, spinach, beans, and dairy. Aim for 2,000-3,000 mg per day.
- Don’t take extra potassium pills unless your doctor tells you to. Even “natural” supplements can be dangerous.
- Stay hydrated. Dehydration concentrates potassium in your blood.
- Know the signs: Muscle weakness, fatigue, irregular heartbeat. If you feel off, get tested.
And here’s the hard truth: most people with hyperkalemia never get dietary counseling. Only 15-20% do. Don’t be one of them. Ask your doctor for a referral to a dietitian who knows kidney and heart conditions.
The Bigger Picture: Don’t Stop Your Meds
For years, the go-to answer for high potassium was to stop the meds. But a 2015 study found that 38% of people on RAASi meds had their dose lowered or stopped because of mild hyperkalemia. That’s a lot of people losing the protection that keeps them alive.
Now we know better. Potassium binders let you keep the benefits of ACE inhibitors and ARBs without the danger. The National Kidney Foundation now recommends binders as first-line treatment for patients who need these drugs.
The future isn’t about choosing between heart health and potassium safety. It’s about managing both. And that’s possible now.
When to Call 911
If you’re on RAASi meds and you suddenly feel:
- Your heart skipping or racing
- Extreme weakness or numbness in your arms or legs
- Difficulty breathing
-go to the ER. Don’t wait. Don’t call your doctor first. Don’t Google it. This isn’t a slow problem. It’s a cardiac emergency.
Can high potassium cause a heart attack?
Yes. High potassium disrupts the heart’s electrical system, which can lead to dangerous arrhythmias like ventricular fibrillation. This stops the heart from pumping blood, which is a cardiac arrest-and if not treated immediately, it’s fatal. Even if it doesn’t cause a classic heart attack from blocked arteries, the result is the same: sudden death.
Can I still take my blood pressure medicine if I have high potassium?
Yes, but you need to manage it. Stopping ACE inhibitors or ARBs increases your risk of death from heart failure or kidney disease. Potassium binders like Veltassa and Lokelma let you keep taking these life-saving drugs while keeping potassium safe. Talk to your doctor about whether a binder is right for you.
How often should I get my potassium checked?
If you’re on RAASi meds or have kidney disease, check every 1-4 weeks after starting or changing your dose. Once stable, every 3-6 months is usually enough. But if you’re sick, dehydrated, or start a new medication, get tested sooner. Don’t wait for symptoms.
Are potassium binders safe for long-term use?
Yes. Both patiromer and sodium zirconium cyclosilicate have been studied for years and are approved for ongoing use. Side effects like constipation or diarrhea are usually mild and manageable. The benefit-staying on your heart and kidney meds-far outweighs the risks for most patients.
What foods should I avoid with high potassium?
Avoid or limit: bananas, oranges, potatoes, tomatoes, spinach, avocados, beans, lentils, dairy products, and salt substitutes. Cooked vegetables can be lower in potassium than raw. Leaching potatoes by soaking them in water can reduce potassium content. A dietitian can help you plan meals that are safe and satisfying.
Can I take over-the-counter supplements if I have hyperkalemia?
No. Many OTC supplements, including multivitamins, protein powders, and herbal products, contain hidden potassium. Even “natural” potassium supplements can be dangerous. Always check with your doctor before taking anything new.
Is hyperkalemia reversible?
Yes, especially if caught early. Acute episodes can be reversed with emergency treatment. Chronic hyperkalemia can be managed long-term with diet, medication adjustments, and potassium binders. The key is consistent monitoring and working with your care team.

