What Heart Failure Really Means - And How It’s Treated Today
Heart failure doesn’t mean your heart has stopped. It means it’s struggling to pump blood the way it should. This isn’t a single disease - it’s a spectrum. Some people have a weak, enlarged heart. Others have a stiff heart that can’t fill properly. The treatment you need depends entirely on which kind you have.
The latest guidelines from the American Heart Association and American College of Cardiology (2023) broke heart failure into two big categories: HFrEF (heart failure with reduced ejection fraction) and HFpEF (heart failure with preserved ejection fraction). If your heart’s pumping ability is below 40%, you’re in the HFrEF group. If it’s 50% or higher, you’re in HFpEF. And there’s a middle ground - HFmrEF - for those between 41% and 49%. This isn’t just semantics. The drugs that work for one group often don’t work for the other.
Stages of Heart Failure: It’s Not Just About Symptoms
Doctors now think of heart failure in four stages, not just ‘mild’ or ‘severe.’
- Stage A: You’re at risk - maybe you have high blood pressure, diabetes, or a family history - but your heart looks normal on scans.
- Stage B: There’s structural damage - a past heart attack, a leaky valve, thickened walls - but you still feel fine.
- Stage C: You have symptoms. Shortness of breath when walking, swelling in your legs, fatigue that won’t quit.
- Stage D: Your heart is failing despite all treatments. You’re in and out of hospitals. Advanced options like devices or transplants are being considered.
This staging matters because treatment changes at each step. In Stage B, starting an ACE inhibitor can cut your risk of developing symptoms by nearly half. In Stage C, you’re not just on one drug - you’re on four, working together.
The New Four-Pillar Treatment for HFrEF
If you have HFrEF, the goal now is quadruple therapy. That’s four classes of drugs, each proven to save lives. And they’re not optional add-ons - they’re the standard.
- ARNI (sacubitril/valsartan): Replaces ACE inhibitors or ARBs. It’s more effective at reducing hospitalizations and death. The number needed to treat to prevent one death over three years? Just 12.
- Heart failure beta blockers: Carvedilol, metoprolol succinate, or bisoprolol. These aren’t your regular blood pressure pills. They’re specifically dosed for heart failure. They slow your heart’s damage over time.
- Mineralocorticoid receptor antagonists (MRAs): Spironolactone or eplerenone. These block a hormone that causes fluid buildup and scarring in the heart.
- SGLT2 inhibitors: Dapagliflozin or empagliflozin. These were originally diabetes drugs. Now they’re frontline heart failure treatments. They reduce hospitalizations by 25% and lower death risk - even if you don’t have diabetes.
Studies show most patients don’t get all four. In fact, only 39% of eligible patients are on the full set within a year of diagnosis. The delay? Often fear of low blood pressure or kidney changes. But real-world data shows severe low blood pressure affects less than 2% of heart failure patients. The biggest barrier isn’t safety - it’s inertia.
HFpEF: The Breakthrough That Changed Everything
For decades, HFpEF had no real drug treatments. Doctors relied on diuretics to drain fluid, but that didn’t touch the underlying problem. Then came the EMPEROR-PRESERVED and DELIVER trials.
Empagliflozin and dapagliflozin - the same SGLT2 inhibitors used in HFrEF - cut hospitalizations for HFpEF by nearly 20%. That’s huge. For the first time, we have drugs that don’t just relieve symptoms - they change the course of the disease.
One patient in Auckland, 72, with HFpEF and type 2 diabetes, started empagliflozin after her third hospitalization in 18 months. Within three months, her walking distance improved by 90 meters. She hasn’t been back to hospital since. That’s not rare anymore. It’s becoming the norm.
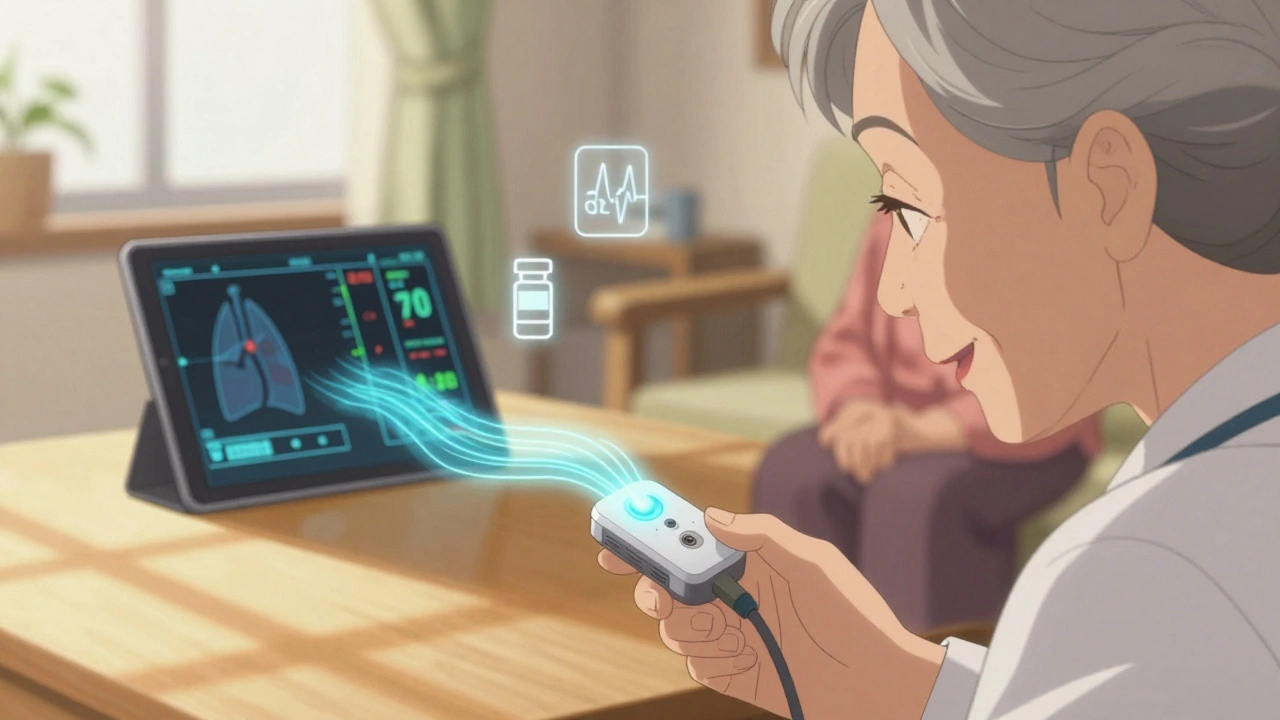
Monitoring Your Heart at Home: The CardioMEMS System
Imagine knowing your heart is starting to fail before you feel it. That’s what the CardioMEMS device does. It’s a tiny sensor implanted in your pulmonary artery during a short procedure. It wirelessly sends pressure readings to your doctor every day.
When pressure rises - even slightly - your care team can adjust your meds before you get swollen, breathless, or end up in the ER. The 2025 MONITOR-HF trial showed a 28% drop in hospitalizations and a big jump in quality of life. Patients report feeling more in control.
It’s not for everyone. It costs around $20,000, and Medicare covers it only for certain high-risk patients. But for those who qualify, it’s life-changing. One woman in Wellington, 68, with recurrent heart failure, said: “I used to dread Tuesdays - that’s when my meds were reviewed. Now I just check my app. If the number’s up, they call me. No more surprises.”
Why Medication Adherence Is the Biggest Hurdle
Getting the right drugs is only half the battle. Taking them correctly is the other half.
The average HFrEF patient takes 7.3 pills a day. Add in meds for diabetes, kidney disease, or atrial fibrillation, and it’s easy to hit 10 or more. One caregiver on HeartFailureMatters.org described managing eight heart meds for her 78-year-old husband: “He forgets which ones to take when. We use a pill organizer, but even then, mistakes happen.”
Studies show 63% of heart failure patients struggle with adherence. The solution? Simplify. Use once-daily formulations. Combine pills where possible. Use smartphone reminders. Ask your pharmacist for a med review. Don’t be afraid to say: “This is too complicated. Can we make it easier?”

Disparities in Care: Who Gets Left Behind
Heart failure care isn’t equal. Black patients are 37% less likely to receive guideline-recommended therapy and 28% more likely to die from it - even after accounting for income, education, or access to care.
Why? Bias, systemic gaps in referral patterns, lack of trust in the system, and underrepresentation in clinical trials all play a role. The ACC’s “HF in a Box” toolkit - used by over 42,000 providers globally - includes patient education materials in 17 languages and checklists designed to reduce these disparities. But tools alone won’t fix it. It takes awareness, advocacy, and accountability.
What’s Next? The Future of Heart Failure Treatment
Research is moving fast. One emerging area is CHIP - Clonal Hematopoiesis of Indeterminate Potential. It’s a blood condition where mutated cells cause inflammation, damaging the heart. It’s found in 15-20% of adults over 70. The INTERCEPT-HF trial is testing if blocking inflammation with canakinumab can help these patients.
Another frontier? Personalized blood pressure targets. We used to aim for 120/80 across the board. Now we’re learning: for HFpEF, keeping systolic pressure above 90 might be safer. For HFrEF, lower targets may be okay. The TARGET-HF trial, tracking 4,200 patients until 2027, will tell us more.
And the market? SGLT2 inhibitors are booming. Farxiga and Jardiance now dominate the HFpEF market. The global heart failure drug market will hit $25 billion by 2029. But money shouldn’t be the focus. The real win is fewer hospital beds filled, more people walking without breathlessness, and longer, better lives.
Living Well With Heart Failure
Heart failure is serious. But it’s not a death sentence. With the right treatment, many people live for years - even decades - with good quality of life.
What helps? Stick to your meds. Monitor your weight daily - a 2kg jump in two days means fluid is building up. Watch your salt. Stay active - even short walks help. Get your flu and pneumonia shots. Sleep with your head up if you’re breathless at night. Talk to your doctor about pulmonary rehab. It’s not just exercise - it’s education, support, and a plan.
One man in Christchurch, 69, with HFrEF, started on quadruple therapy after his second hospitalization. He’s now hiking with his grandchildren. “I used to think this was the end,” he said. “Now I know it’s just a new beginning.”