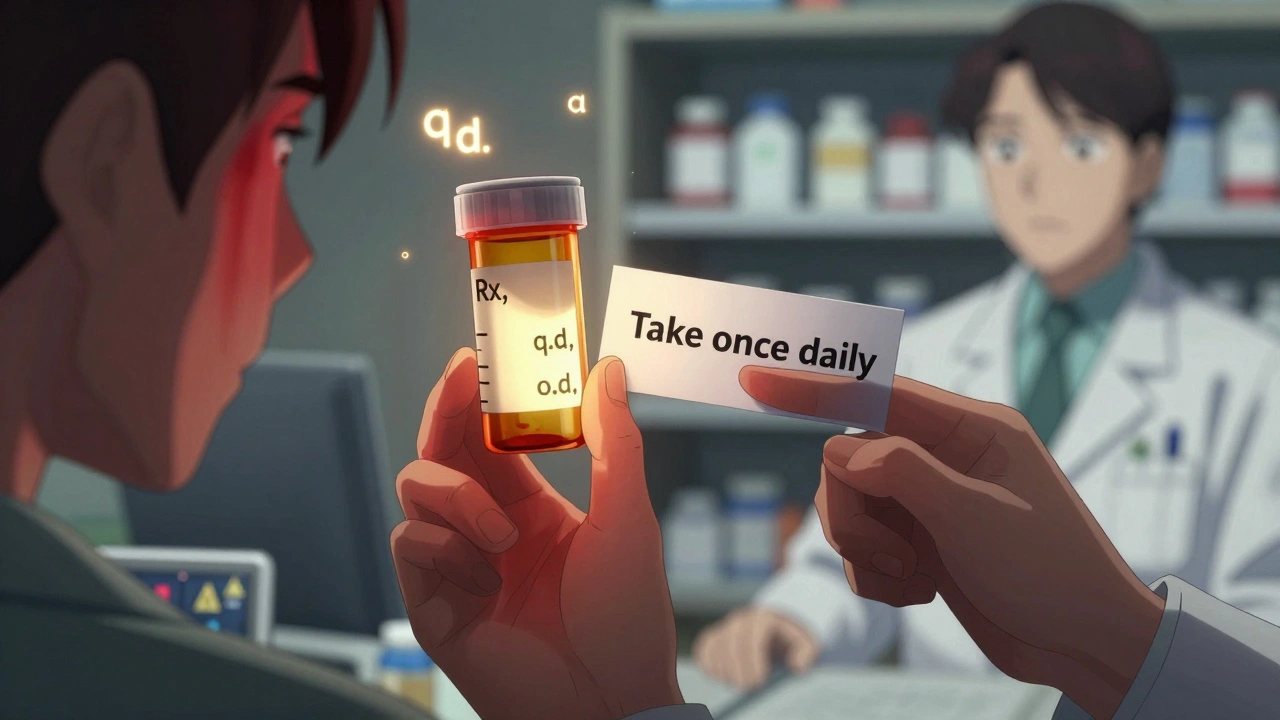
Ever stared at your prescription label and felt like you’re reading a secret code? That little Rx on top? The q.d. or b.i.d.? The tiny o.d. or a.s.? You’re not alone. These aren’t just random letters-they’re shorthand used by doctors and pharmacists for over 400 years. But in today’s world, where one wrong symbol can lead to a dangerous mistake, understanding them isn’t just helpful-it’s critical.
What Does Rx Really Mean?
The Rx symbol you see at the top of every prescription? It’s not a brand logo or a random design. It comes from the Latin word recipe, which means "take." Back in the 1500s, doctors wrote prescriptions in Latin so they’d be understood across Europe. Today, it’s still used because it’s quick, but it’s also one of the few Latin terms still allowed everywhere. You’ll see it on every bottle, every digital script, every pharmacy screen. It’s the universal starting point: "Take this."
But here’s the problem: while Rx is safe, many other abbreviations are not. The Joint Commission, which sets safety standards for U.S. hospitals, has a list of 12 abbreviations that are banned because they’ve caused deaths. One of them? U for units. A handwritten U can look like a 4 or even a 0. In Pennsylvania alone, between 2018 and 2022, 12 people died because someone misread U as something else. That’s why today, every pharmacy in the U.S. is required to write out "units" in full.
Common Dosage Abbreviations and Why They’re Dangerous
Let’s break down the most common ones you’ll see on your label:
- q.d. = once daily
- b.i.d. = twice daily
- t.i.d. = three times daily
- q.i.d. = four times daily
- q.o.d. = every other day
These all come from Latin. But here’s the catch: q.d. looks a lot like q.i.d.. One letter changes everything. In 2021, the Institute for Safe Medication Practices found that q.d. was misread as q.i.d. in over 21% of all frequency-related errors. That means someone meant to take a pill once a day-and ended up taking it four times. That’s how overdoses happen.
Because of this, most pharmacies now convert q.d. to "daily," b.i.d. to "twice a day," and so on. If your label says "daily," that’s intentional. It’s safer. If you still see q.d. on your script, ask your pharmacist to confirm what it means. Don’t assume.
Eye and Ear Abbreviations: A Silent Killer
One of the most dangerous sets of abbreviations has nothing to do with dosage. It’s about where the medicine goes. Take these:
- o.d. = right eye (oculus dexter)
- o.s. = left eye (oculus sinister)
- a.d. = right ear (auris dexter)
- a.s. = left ear (auris sinister)
These are used for eye drops, ear drops, and even some glaucoma medications. But here’s the trap: o.d. looks like "OD," which everyone knows means "overdose." In 2022, the American Academy of Ophthalmology reported that 12.3% of eye medication errors came from this confusion. One patient got eye drops meant for their right eye-but took them in their left eye because the label was misread as "overdose" and they thought they’d been given the wrong bottle.
Worse, a.d. and a.s. are often confused with o.d. and o.s. by pharmacists rushing through prescriptions. A 2023 study found that 19.3% of community pharmacy errors involved mixing up eye and ear directions. That’s why smart pharmacies now write out "right eye," "left ear," and so on-no abbreviations.
What About MS, SC, and IU?
Some abbreviations look harmless but can be deadly.
- MS could mean morphine sulfate-or magnesium sulfate. These are two completely different drugs. One calms pain. The other treats seizures. Mixing them up can kill.
- SC means subcutaneous (under the skin). But if it’s handwritten poorly, it can look like SL (sublingual, under the tongue). Giving insulin sublingually instead of under the skin? That’s a medical emergency.
- IU stands for international units. But it can be mistaken for "IV" (intravenous). Giving a drug meant to be injected into the skin through a vein? That’s dangerous.
These aren’t theoretical risks. The American Hospital Association documented over 14,000 incidents in 2023 alone. The most common? OD misread as overdose (2,147 cases), SC misread as SL (1,873 cases), and 1.0 mg misread as 10 mg (1,562 cases). That last one? It’s why hospitals now require leading zeros-0.5 mg, never .5 mg. A missing zero can mean a 10x overdose.
How Pharmacies Are Fixing This
Thankfully, the system is changing. Most major pharmacies-CVS, Walgreens, Walmart-now have strict rules:
- Every prescription is scanned by software that flags banned abbreviations.
- Pharmacists must review every script manually before handing it out.
- Patient labels are rewritten in plain English: "Take one tablet by mouth twice a day," not "1 tab p.o. b.i.d."
Electronic prescribing systems like Epic and Cerner now auto-convert old abbreviations. If a doctor types q.d., the system changes it to "daily" before it even reaches the pharmacy. In hospitals using these systems, abbreviation-related errors dropped by 43%.
But here’s the catch: not everyone uses electronic systems. Some doctors still write prescriptions by hand. Some clinics use old software. That’s why 67.8% of community pharmacies still see dangerous abbreviations every week.

What You Should Do
You don’t need to memorize all 487 abbreviations. But you do need to be your own safety net.
- Always ask if you see an abbreviation you don’t recognize. Don’t be shy. "What does this mean?" is the most powerful question you can ask.
- Check your label. If it says "q.d." or "o.d.", ask the pharmacist to rewrite it in plain English. Most will do it without hesitation.
- Compare the script to the bottle. If the instructions don’t match what your doctor told you, speak up.
- Use the pharmacy’s app. Most chains now let you view your prescriptions online. Look for the "Patient Instructions" section-it’s usually in plain English.
- Keep a list. Write down the meaning of any abbreviation your doctor uses often. Bring it to every appointment.
One pharmacist in New Zealand told me about a patient who took eye drops meant for her right eye in both eyes because the label said "o.d." She thought it meant "both eyes." She didn’t know Latin. She didn’t need to. All she needed was a pharmacist who took five seconds to write "right eye" instead.
The Future Is Plain Language
The World Health Organization wants all prescriptions to use English-only terms by 2030. Australia, Canada, and Germany are already there. The U.S. is catching up. By 2027, experts predict 95% of electronic prescriptions will have no Latin abbreviations left.
Why? Because safety isn’t about tradition. It’s about survival. The old system worked when doctors and pharmacists spoke Latin. Today, we speak English. And when it comes to your health, clarity beats speed every time.
If your prescription says "b.i.d.," ask for "twice a day." If it says "o.s.," ask for "left eye." If it says "U," ask for "units." You’re not being difficult. You’re being smart. And in a world where a single letter can change your life, that’s not just good advice-it’s essential.