Keeping emergency medications like epinephrine, naloxone, or nitroglycerin both accessible and secure isn’t just a good idea-it’s a lifesaving balance. Too locked up, and you risk delays during a cardiac arrest or opioid overdose. Too loose, and a curious child, a visitor, or even a thief could get to them. The stakes are high, and the solution isn’t one-size-fits-all. Whether you’re storing these meds at home, in a school, or in an EMS vehicle, the goal is the same: get the right drug to the right person in seconds, without letting it fall into the wrong hands.
Know What You’re Storing
Not all emergency medications are the same. Epinephrine auto-injectors (like EpiPens) must stay at room temperature-between 20°C and 25°C (68°F-77°F). Refrigerating them can damage the device and reduce effectiveness. Naloxone nasal spray (Narcan) also prefers room temperature, though some formulations can tolerate brief cold exposure. Nitroglycerin tablets, on the other hand, are sensitive to heat and light and should be kept in their original glass bottle, tightly closed, away from direct sunlight. Mixing these up in storage can lead to ineffective drugs when you need them most.Check the label. Only 43% of prescription bottles include clear storage instructions, according to the FDA’s 2022 review. Don’t assume. If it’s not clear, call the pharmacy. A degraded epinephrine injector won’t save a life-and you won’t know until it’s too late.
Home Storage: Lock It, But Not Too Tight
At home, the biggest risks are children and accidental misuse. The EPA recommends storing all medications in locked cabinets, closets, or safes. But for emergency drugs, that lock can’t be a barrier. A combination lock or key lock on a high shelf? That’s dangerous. If you’re using naloxone for someone at risk of overdose, you need it reachable within 10 seconds-no fumbling with keys or codes.Here’s what works: use a small, wall-mounted medicine safe with a quick-access keypad or thumbprint lock. These are commercially available for under $50 and are designed for exactly this purpose. Or, if you don’t want to buy one, use a locked drawer in a bedroom dresser-not the bathroom or kitchen. Keep it out of sight but within arm’s reach of the person who needs to access it. Label it clearly: “Naloxone - Emergency Use Only.”
For families with kids, store routine medications (like painkillers or antibiotics) in a separate, locked container. Emergency meds? Keep them in their own space. The American Academy of Pediatrics says this separation reduces accidental exposure by up to 70%.
Workplaces and Schools: Access Without Compromise
Schools and workplaces often keep epinephrine or naloxone on hand for staff or visitors. The rules here are stricter than at home. In New Zealand, the Ministry of Health recommends storing emergency medications in a clearly labeled, locked box with a key held by trained staff-usually the school nurse, office manager, or designated first aid responder.But here’s the catch: that key must be carried, not left in a drawer. During drills or emergencies, every second counts. Many schools now use wall-mounted lockboxes with push-button codes known only to trained personnel. These are tamper-evident, weather-resistant, and can be mounted near entrances, cafeterias, or sports fields.
Don’t store emergency meds in unlocked first aid kits. That’s a common mistake. A 2023 study in the American Journal of Health-System Pharmacy found that 41% of schools kept epinephrine in unlocked containers, leading to expired or missing doses. Training matters too. Staff should practice accessing the medication every three months. Competency checks improve response time by over 50%.
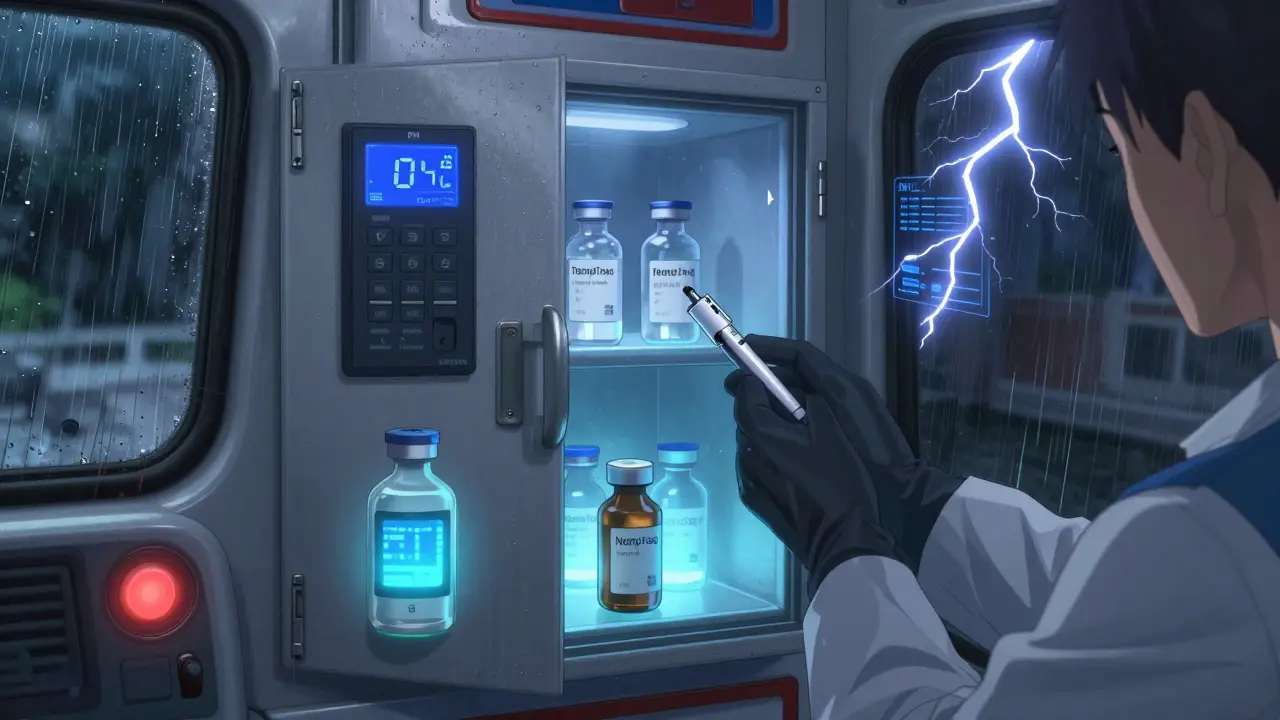
EMS and Vehicles: Mobile, Secure, and Monitored
In ambulances and emergency vehicles, medications are stored in lockable cabinets that meet DEA standards for controlled substances. Schedule II drugs like morphine must be kept separate from other meds in a double-locked container. But here’s the twist: the cabinet must open in under 15 seconds-even with gloves on, in a moving vehicle, during a storm.Modern EMS units use electronic lockboxes with biometric or PIN access, synced to the vehicle’s GPS and logging every opening. Temperature monitoring is non-negotiable. A 2023 report from Nevada EMS found 32% of EMS agencies had at least one temperature excursion during extreme weather. That means epinephrine or insulin could be ruined before it’s even used.
Portable devices like TempTraq (FDA-approved) stick to medication containers and send alerts if temps go outside 2°C-8°C for refrigerated drugs or 15°C-30°C for room-temp meds. Some systems even send text alerts to supervisors. This isn’t luxury-it’s standard in top-tier services.

Special Cases: Operating Rooms and Nursing Homes
In hospitals, especially operating rooms, emergency meds are often kept in open, clearly labeled drawers-right next to the anesthesia cart. Why? Because in a code blue, you don’t have time to unlock anything. The American Society of Anesthesiologists allows this only if the area is under constant visual supervision by licensed staff.In nursing homes, where residents may have dementia or cognitive decline, locked cabinets are still required-but access must be fast. Many facilities use keypads with individual codes for nurses, or smart cabinets that unlock only when a nurse swipes their badge. Some even integrate with electronic health records: if a patient’s vitals drop, the cabinet unlocks automatically for the assigned caregiver.
Temperature and Condition Checks: Don’t Ignore the Details
Medications don’t just need to be secure-they need to be effective. Heat, moisture, and light degrade them. Epinephrine loses potency after just 30 days at 35°C. Naloxone can become ineffective if exposed to freezing temps.Here’s a simple routine: check your emergency meds every 30 days. Look for discoloration, cloudiness, or particles. If the auto-injector’s window isn’t clear, replace it. Keep a log. Use a small notepad or a phone app. If you’re in a hot climate like Auckland’s summer, avoid storing meds in cars or near windows. Even a garage can hit 40°C on a sunny day-way above the safe limit.
Training and Drills: Practice Makes Lifesaving
You can have the best lockbox in the world, but if no one knows how to open it fast, it’s useless. A 2023 study showed that after two 90-minute training sessions, 85% of healthcare workers could access emergency meds in under 12 seconds. Without training, that number drops to 28%.Practice with your family. Show your partner, teen, or neighbor how to use naloxone. Don’t wait for an emergency to learn. Use training kits-many pharmacies give them out free. The CDC’s PROTECT Initiative says: “Never leave medicine out on a kitchen counter. Put medicines away every time.” That applies to homes, schools, and workplaces alike.
What to Avoid
- Don’t store emergency meds in the bathroom. Humidity ruins them.
- Don’t rely on “I’ll remember where I put it.” Use a fixed, labeled spot.
- Don’t mix emergency meds with daily pills. Confusion leads to errors.
- Don’t assume a locked box means safe. If it takes more than 15 seconds to open, it’s not emergency-ready.
- Don’t ignore expiration dates. Epinephrine auto-injectors expire in 12-18 months. Replace them on time.
Future Tech: Smarter Storage Is Coming
By 2027, Gartner predicts 65% of healthcare facilities will use AI-powered storage systems that adjust access based on real-time risk. Imagine a cabinet that unlocks only when a patient’s heart rate drops below a threshold-or when a caregiver’s fingerprint is scanned during a crisis. These systems are already being tested in New Zealand hospitals.For home users, smart locks with voice activation (like “Unlock naloxone”) are on the horizon. But for now, the best tech is simple: a reliable lockbox, a clear plan, and people who know how to use it.
Can I keep emergency medication in my car?
No. Cars get too hot in summer-often above 40°C (104°F)-which can destroy epinephrine, insulin, or nitroglycerin. Even in winter, freezing temps can damage some formulations. Always store emergency meds indoors, in a stable environment.
What if I’m traveling with emergency meds?
Carry them in your hand luggage. Keep them in their original packaging with the prescription label. Use a small insulated pouch with a cold pack if needed for refrigerated drugs-but never freeze them. For epinephrine or naloxone, room temperature is fine. Never check them in baggage; delays or temperature swings can ruin them.
How do I dispose of expired emergency meds?
Never flush them or throw them in the trash. Take expired epinephrine, naloxone, or other controlled substances to a pharmacy with a take-back program. In New Zealand, most pharmacies offer free disposal. If none are nearby, mix the meds with coffee grounds or cat litter, seal them in a container, and put them in the trash. Remove personal info from labels first.
Is it legal to keep naloxone at home without a prescription?
Yes. In New Zealand, naloxone is available over the counter at pharmacies without a prescription. Many pharmacies offer it for free through public health programs. You don’t need to be a doctor or have a patient to keep it. If you know someone at risk of opioid overdose, having naloxone at home is not just legal-it’s responsible.
What’s the difference between a medicine safe and a regular lockbox?
A medicine safe is built to resist tampering, moisture, and temperature extremes. Regular lockboxes may be flimsy plastic or thin metal that can be pried open. Look for safes labeled as “pharmaceutical-grade” or “tamper-evident.” Many have alarms, logs, or temperature sensors. For emergency use, you need durability-not just a lock.
Final Checklist
- ✅ Know the correct storage temp for each emergency med.
- ✅ Store meds in a fixed, labeled, locked location-not a drawer or purse.
- ✅ Train at least two people in your household or workplace how to access and use them.
- ✅ Check expiration dates every 30 days.
- ✅ Replace expired or discolored meds immediately.
- ✅ Use a temperature monitor if you’re in extreme climates.
- ✅ Know where to dispose of expired meds safely.
Emergency meds aren’t just pills or devices-they’re time-sensitive tools. Their value isn’t in how well they’re locked away, but in how quickly they can be used. The right balance isn’t about locking tighter-it’s about locking smarter.

