Why your prescription costs less in the U.S. than in Canada - but your brand-name pills cost way more
If you’ve ever compared your pharmacy receipt to a friend’s from Europe or Australia, you might’ve been surprised. You paid less for your generic blood pressure pill than they did - but your insulin? That cost three times as much. The U.S. doesn’t just have high drug prices. It has two very different drug markets. One is cheap. The other is shockingly expensive. And most people don’t even realize it.
Here’s the truth: 90% of prescriptions filled in the U.S. are generics. And for those, you’re often paying less than people in nearly every other developed country. But the other 10%? The brand-name drugs? Those are the ones that drag the whole system into the red. Americans pay more for those than anyone else on Earth.
Generic drugs: U.S. prices are actually the lowest
Let’s start with the good news. If you’re taking a generic version of metformin, lisinopril, or atorvastatin, you’re getting one of the best deals in the world. According to a 2022 study by the RAND Corporation, U.S. prices for unbranded generic drugs were 33% lower than the average in 33 other wealthy nations. That means for every $1 spent on a generic pill in Germany or Japan, you paid about 67 cents in the U.S.
Why? Three big reasons. First, the U.S. fills over 90% of prescriptions with generics. That kind of volume gives pharmacies and insurers massive negotiating power. Second, the FDA approves generics fast. When three or more companies start making the same drug, prices crash - often down to 15-20% of the original brand’s price. Third, public programs like Medicare Part D and Medicaid don’t pay list prices. They negotiate deep discounts.
Take the diabetes drug metformin. In 2023, the average U.S. cash price for a 30-day supply was $4. Some pharmacies sold it for $1. In the U.K., the same dose cost about $7. In France, $9. In Canada, $11. Yet Americans still hear that U.S. drug prices are the highest. That’s because they’re thinking of insulin, not metformin.
Brand-name drugs: The U.S. is the outlier
Now flip the script. For brand-name drugs, the U.S. is the most expensive country in the world. A 2023 report from the Department of Health and Human Services found that U.S. prices for originator drugs - the original, patent-protected versions - were 422% higher than in other OECD countries. That’s more than four times the price.
Take Jardiance, a diabetes drug. Medicare negotiated a price of $204 for a 30-day supply. In Japan? $52. In Australia? $48. In Germany? $61. The same drug, same manufacturer, same clinical data - but in the U.S., you pay nearly four times more.
Why does this happen? Unlike most countries, the U.S. doesn’t set drug prices. Pharmaceutical companies set their own list prices. Insurers and pharmacy benefit managers negotiate rebates behind closed doors. That means the price you see on the shelf - or the price a hospital pays - isn’t the real price. But if you’re uninsured, or your plan has a high deductible, you pay that list price. And that’s where the pain hits.

What’s really going on with net vs. list prices
Here’s where it gets confusing. A 2024 study from the University of Chicago found that when you look at net prices - what the government and insurers actually pay after rebates - the U.S. is cheaper than Canada, Germany, and the U.K. That’s because those countries don’t have the same rebate system. They set a single price, and everyone pays it.
In the U.S., the list price is like a sticker on a car. The dealer offers discounts, cashback, trade-ins. You only pay the final price if you’re savvy enough to negotiate. But if you’re not insured, or your insurance doesn’t cover the rebate, you pay the sticker price. That’s why a person with Medicare Part D might pay $20 for a drug, while an uninsured person pays $200 for the same thing.
The result? Two Americas. One where generics are dirt cheap and brand-name drugs are negotiated down. Another where people pay full price - and that’s where the outrage comes from.
How competition drives down generic prices
There’s a simple rule in generic drug pricing: more companies = lower prices. When the first generic version of a drug hits the market, it’s usually 35-40% cheaper than the brand. Add a second company? Prices drop another 20%. By the time three or four manufacturers are making it, prices fall to 15-20% of the original.
But here’s the catch: sometimes, too many companies leave the market. If the price drops too low, manufacturers stop making the drug because it’s not profitable. Then, only one company is left. And guess what? They raise the price. That’s what happened with doxycycline in 2013. A generic antibiotic that once cost $20 a bottle jumped to $1,800 after two manufacturers left the market. It took years for competition to return.
The FDA now tracks these “generic drug shortages” closely. Their 2023 report showed that 773 new generic approvals that year could save the system $13.5 billion. That’s the power of competition. But it only works if the market stays crowded.
Medicare’s new drug negotiations: Still higher than everywhere else
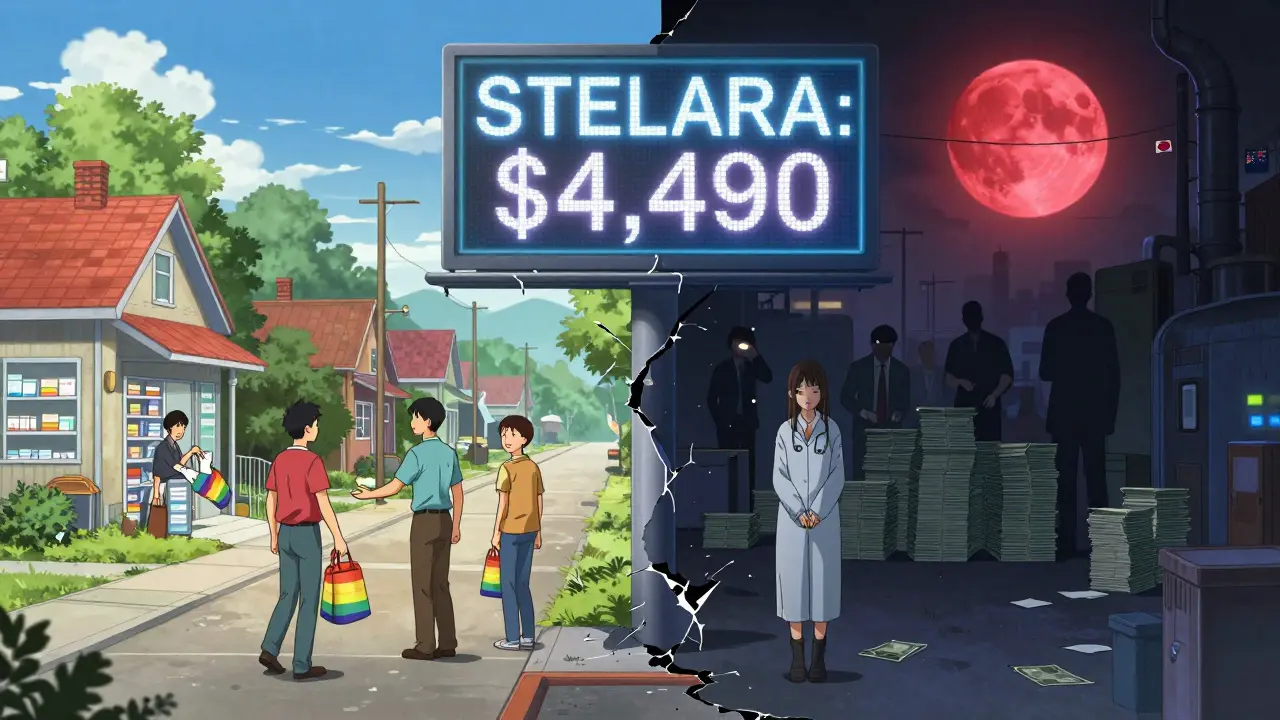
In 2022, Congress gave Medicare the power to negotiate prices for the most expensive drugs. The first 10 drugs were announced in 2023. The results? Even after negotiation, Medicare’s prices are still higher than what other countries pay.
For Stelara, a psoriasis drug, Medicare’s negotiated price was $4,490 per dose. In Germany? $2,822. In Japan? $2,100. In Australia? $1,900. In every case except one, the U.S. government still paid more than foreign governments - even after bargaining.
That’s not a failure of negotiation. It’s a sign of how high U.S. brand-name prices started. Medicare didn’t bring prices down to global levels. It just brought them down from the moon.
What this means for you
If you’re taking a generic, you’re winning. You’re paying less than most people in the world. Use GoodRx. Compare prices. Buy 90-day supplies. These are smart moves - and they work.
If you’re on a brand-name drug, especially one with no generic, you’re in the tough spot. Ask your doctor: Is there a similar drug that’s generic? Can I switch? Can I get a patient assistance program? Many drugmakers offer discounts for low-income patients. Don’t assume you’re stuck with the price tag.
And if you’re uninsured or underinsured? Know this: the U.S. system is designed to protect the insured. If you’re outside that safety net, you’re paying the highest price in the world. That’s not fair. But it’s real.
Why the world pays less - and what that means for innovation
Pharmaceutical companies argue that high U.S. prices fund global innovation. That’s true - to a point. The U.S. pays more for research, and other countries get the benefit. That’s why some experts say the U.S. is subsidizing the rest of the world.
But here’s the twist: the U.S. doesn’t pay more for generics. We pay less. And generics don’t fund R&D. Only brand-name drugs do. So if we cut brand-name prices to global levels, innovation might slow. But if we keep them this high, millions of Americans can’t afford their meds.
There’s no easy fix. But one thing is clear: the U.S. doesn’t have a drug pricing problem. It has a two-tier problem. One tier works. The other doesn’t. And until we fix the broken one, no amount of generic savings will make the system fair.
Are generic drugs in the U.S. really cheaper than in other countries?
Yes. For unbranded generic drugs, U.S. prices are about 33% lower than the average in 33 other wealthy countries, according to a 2022 RAND Corporation study. For common generics like metformin or lisinopril, you often pay $1-$6 in the U.S., while the same drugs cost $7-$15 in Canada, Germany, or the U.K.
Why are brand-name drugs so expensive in the U.S.?
The U.S. doesn’t regulate drug prices. Companies set their own list prices, and insurers negotiate rebates behind the scenes. Other countries set price caps. In the U.S., if you’re uninsured or have a high deductible, you pay the full list price - which can be 4 times higher than what other countries pay for the same drug.
Does Medicare negotiate lower prices for drugs?
Yes, but not low enough. Medicare’s first 10 negotiated drug prices in 2023 were still 1.6 to 3.9 times higher than prices in countries like Japan, Australia, and Germany. The program saved money compared to U.S. list prices, but it didn’t bring prices down to global levels.
Why do some generic drugs suddenly become very expensive?
When too many manufacturers stop making a generic drug - because the price is too low - only one or two companies remain. That creates a monopoly. Without competition, prices spike. This happened with doxycycline and minocycline, where prices jumped over 1,000% after manufacturers left the market.
Can I save money on generic drugs in the U.S.?
Absolutely. Use GoodRx or SingleCare to compare prices across pharmacies. Buy 90-day supplies instead of 30-day. Ask if your pharmacy has a $4 generic list. Many generics cost less than $10 - sometimes under $5 - even without insurance. The U.S. has the cheapest generics in the world; you just need to know where to look.
Why do other countries pay less for the same brand-name drugs?
Most countries have government agencies that set price limits. They negotiate with drugmakers as a single buyer. The U.S. has hundreds of insurers, each negotiating separately. That gives drugmakers more leverage. Countries like Japan and France also cap profits and require companies to justify price increases.

