MH Treatment Timing Calculator
Time is critical in malignant hyperthermia. Every minute counts for survival. See how treatment timing affects outcomes based on the latest medical research.
Key Time Windows
• 0-20 minutes: Treatment highly effective. Survival rate >95%
• 20-40 minutes: Treatment less effective. Survival rate ~50%
• 40+ minutes: Treatment becomes ineffective. Survival rate <50%
Important Medical Note
Dantrolene is the only treatment that stops the calcium flood in muscle cells. Survival depends on getting dantrolene within 20 minutes of the first sign. After 40 minutes, survival chances drop significantly.
Survival Rate
Based on latest clinical data from the Malignant Hyperthermia Association of the United States
When you walk into a hospital for surgery, you expect to be safe. But for a small number of people, a routine anesthetic can trigger a terrifying, fast-moving crisis called malignant hyperthermia. It doesn’t happen often-about 1 in every 5,000 to 100,000 procedures-but when it does, every second counts. This isn’t a fever or a bad reaction to drugs. It’s a genetic emergency where your muscles go into overdrive, your body temperature spikes dangerously high, and your organs start to shut down-all within minutes.
What Exactly Is Malignant Hyperthermia?
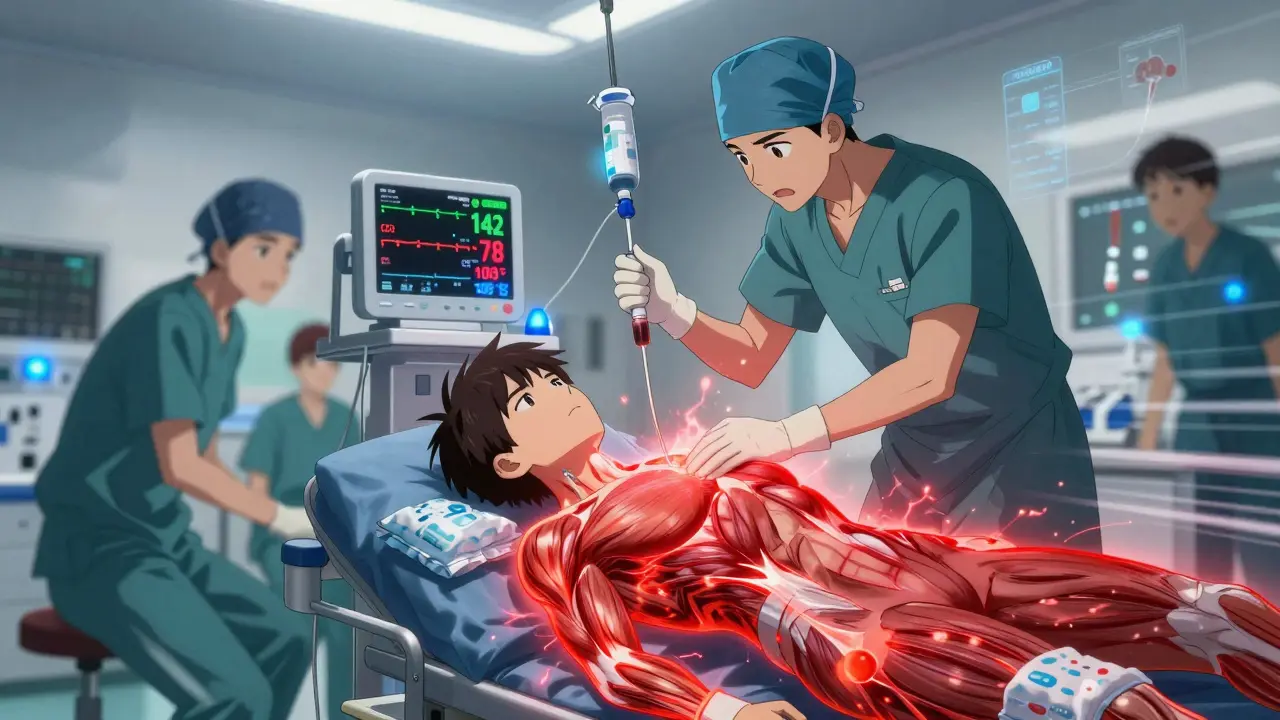
Malignant hyperthermia (MH) is a rare but deadly condition triggered by specific anesthetic drugs in people with a hidden genetic mutation. It’s not an allergy. It’s not an overdose. It’s a flaw in how muscle cells handle calcium. Normally, calcium is stored safely inside muscle cells until the brain signals a movement. In MH-susceptible individuals, certain anesthetics cause that calcium to flood out uncontrollably. The muscles lock up, burn through oxygen like wildfire, and produce massive amounts of heat. Core body temperature can climb from normal to over 109°F (43°C) in under an hour.The two main triggers are volatile anesthetic gases-like sevoflurane, desflurane, and isoflurane-and the muscle relaxant succinylcholine. These are common in surgeries from tonsillectomies to heart operations. About 70% of MH cases are linked to mutations in the RYR1 gene on chromosome 19. Another 1% involve the CACNA1S gene. These mutations run in families, but many people never know they carry them until they’re exposed to anesthesia.
How Do You Know It’s Happening?
The signs don’t wait. They show up fast, often within the first 30 minutes after the anesthetic starts. Early warning signs include:- A sudden, unexplained spike in heart rate-over 120 beats per minute
- Rapid breathing and rising carbon dioxide levels (end-tidal CO2 above 55 mmHg)
- Stiff jaw muscles (masseter spasm), especially after succinylcholine
- Dark, cola-colored urine, a sign of muscle breakdown
- Body temperature rising above 104°F (40°C)
These symptoms are easy to miss if you’re not looking for them. A rising heart rate might be chalked up to pain or anxiety. High CO2 might seem like poor ventilation. But in an operating room, these are red flags. Anesthesiologists are trained to spot them. One doctor on Reddit described catching MH at 32 minutes into a procedure when CO2 hit 78 mmHg and heart rate jumped to 142 in a previously stable 28-year-old man. That’s the kind of moment that saves lives.
Why Timing Is Everything
The difference between life and death comes down to minutes. Before dantrolene was available in the 1970s, 80% of MH cases were fatal. Today, with prompt treatment, mortality has dropped to about 5%. But that only works if dantrolene is given within 20 minutes of the first sign. If treatment is delayed beyond 40 minutes, survival chances drop to 50%.Dantrolene is the only drug that directly stops the calcium flood in muscle cells. It’s not a miracle cure-it’s a targeted rescue. The standard dose is 2.5 mg per kilogram of body weight, given intravenously. If symptoms don’t improve, you repeat the dose every 5 to 10 minutes, up to a maximum of 10 mg/kg. That’s often 20 to 40 vials in a single case.
There are two versions: Dantrium® and Ryanodex®. Ryanodex, approved in 2014, dissolves in just one minute instead of 22. That’s huge in an emergency. Each vial costs around $4,000. Hospitals are required to keep at least 36 vials on hand-$144,000 worth of emergency medicine, just in case.
What Happens After Dantrolene?
Giving dantrolene isn’t the end of the story. The body is in chaos. You need to:- Stop all triggering anesthetics immediately
- Give 100% oxygen at 10 liters per minute
- Cool the patient aggressively-ice packs on neck, armpits, groin, and cold IV fluids
- Treat acidosis with sodium bicarbonate
- Manage high potassium with insulin and glucose
- Protect the kidneys with mannitol and furosemide to flush out muscle breakdown products
Without these steps, even if dantrolene works, the patient can still die from kidney failure, heart rhythm problems, or blood clotting issues. The damage from rhabdomyolysis-where muscle tissue melts into the bloodstream-can linger for days.
Who’s at Risk? And Why Most People Don’t Know
You might think MH only affects people with a family history. But new research shows 29% of cases happen in people with no known relatives who’ve had it. That means if you’ve never had a bad reaction to anesthesia, you’re not necessarily safe.Surveys show 68% of MH survivors had never heard of the condition before their own crisis. Many patients report being told they were “just unlucky” or “had a bad reaction.” That’s not luck. It’s a genetic condition that’s been missed.
There’s a test-called the caffeine-halothane contracture test (CHCT)-that can confirm MH susceptibility. It requires a muscle biopsy and is only done at specialized centers. Genetic testing for RYR1 mutations is now available too, with 95% accuracy for known variants. But it’s expensive-$1,200 to $2,500-and not routinely offered unless there’s a family history or prior reaction.

How Hospitals Are Preparing
Leading hospitals have turned MH preparedness into a science. At Mayo Clinic, they keep full MH emergency carts-stocked with dantrolene, cooling supplies, syringes, and IV fluids-within 30 seconds of every operating room. Before 2015, it took an average of 22 minutes to get dantrolene ready. Now, it’s under 5 minutes. That’s what saved lives.Every hospital performing general anesthesia in the U.S. is now required by the FDA to have an MH emergency kit. But compliance varies. Academic hospitals are nearly 100% ready. Rural centers? Only 63%. Some report stockouts. Others don’t train staff annually. That’s dangerous.
Training is non-negotiable. Anesthesiology residents need at least three simulation drills to reliably recognize MH. The Malignant Hyperthermia Association of the United States (MHAUS) runs a 24/7 hotline (1-800-644-9737) for real-time advice during crises. Since 1997, that line has helped cut mortality by 37%.
What’s Next?
The future is promising. In 2023, the FDA approved a new intranasal form of dantrolene for emergency use outside the hospital-expected to hit the market in mid-2024. That could help in ambulances or ERs. Researchers are also testing drugs like S107 that stabilize the ryanodine receptor, potentially preventing MH before it starts. Long-term, CRISPR gene editing might one day fix the RYR1 mutation itself. Phase I trials are projected for 2027.Right now, the biggest change is happening in anesthesia machines. Epic Systems’ 2024 software update now includes real-time MH detection. If a patient’s CO2 rises above 55 mmHg, heart rate exceeds 120, and temperature goes over 104°F-all at once-the system auto-alerts the team. No more relying on a single person to spot subtle signs.
What You Should Do
If you’ve had a bad reaction to anesthesia-or if a close relative has-you should get tested. Tell your anesthesiologist before any surgery. Ask if the facility has dantrolene on hand and if staff do annual MH drills. Don’t assume it’s covered. If you’re scheduled for a tonsillectomy or any surgery under general anesthesia, especially as a child, ask about MH protocols.It’s not paranoia. It’s prevention. For most people, anesthesia is perfectly safe. But for those with the mutation, knowing the signs and demanding preparedness can mean the difference between walking out of the hospital-or not.
Can malignant hyperthermia be cured?
There is no cure for the genetic mutation that causes malignant hyperthermia. But the reaction itself can be stopped with immediate treatment-primarily dantrolene-and most patients recover fully if treated within 20 minutes. Long-term, survivors need monitoring for muscle and kidney issues, but they can live normal lives with proper precautions during future surgeries.
Is malignant hyperthermia hereditary?
Yes, it’s inherited in an autosomal dominant pattern. If one parent has the mutation, each child has a 50% chance of inheriting it. But not everyone with the mutation will react to anesthesia-some never get exposed. That’s why many cases go undetected until a family member has a crisis. Genetic testing can identify carriers.
Can you have malignant hyperthermia without anesthesia?
Extremely rare, but possible. There are isolated reports of MH-like episodes triggered by extreme heat, intense exercise, or seizures in genetically susceptible people. These are called exertional or heat-related MH variants. They’re not the same as anesthesia-triggered MH, but they share the same underlying muscle defect. People with known mutations should avoid extreme physical stress and overheating.
What if I’m allergic to dantrolene?
True allergies to dantrolene are nearly unheard of. The drug has been used safely for over 50 years. If you’ve had a reaction to another medication, tell your anesthesiologist-but don’t assume it’s a dantrolene allergy. In a true MH crisis, there are no alternatives. Delaying dantrolene is far more dangerous than any theoretical allergic risk.
Do all anesthesiologists know how to handle malignant hyperthermia?
They’re trained to, but real-world readiness varies. Hospitals with academic affiliations and high surgical volumes typically have strong protocols and annual drills. Smaller or rural facilities may lack resources or training. Always ask: “Do you have dantrolene on-site? Do you practice MH drills?” If the answer is vague, consider transferring care to a better-equipped center.
Can I be tested for malignant hyperthermia before surgery?
Yes, if you have a family history of MH or a prior unexplained reaction. Genetic testing for RYR1 mutations is available through certified labs and costs $1,200-$2,500. The gold standard is the muscle biopsy test (CHCT), but it’s invasive and only done at a few specialized centers. Testing isn’t routine, but it’s critical for at-risk individuals.
Is succinylcholine the only muscle relaxant that triggers MH?
Succinylcholine is the most common muscle relaxant trigger, but it’s not the only one. Other depolarizing agents can also cause MH, though they’re rarely used today. Non-depolarizing muscle relaxants like rocuronium or vecuronium are considered safe. If you’re MH-susceptible, your anesthesiologist will avoid succinylcholine and use safer alternatives.
What should I do if I suspect someone is having malignant hyperthermia?
Call for help immediately. If you’re in a hospital, alert the anesthesiologist and surgical team. If you’re outside a medical setting and someone collapses with high fever, muscle rigidity, and rapid breathing after anesthesia, call 911 and state, “Suspected malignant hyperthermia.” Time is critical. Don’t wait. Every minute counts.