Medication List Generator
Your Medication List
Create a complete medication list for your doctor appointment. Include all prescription medications, supplements, and over-the-counter drugs. This helps prevent errors and ensures your doctor has the full picture of your health.
Walking into a doctor’s office without being prepared is like showing up to a job interview without a resume. You might have all the right answers in your head, but if you can’t clearly explain what’s going on, the doctor won’t have the full picture. And that’s dangerous. Studies show that patients who prepare ahead of time have 31% higher appointment productivity and are 89% more likely to get their main health concerns fully addressed.
What to Bring: The Must-Have List
You don’t need to bring everything you own. But you do need to bring the right things. Missing one item can delay your care-or worse, lead to a wrong diagnosis.
- Medication list: Not just the names. Write down the exact drug, strength (like "15mg"), how often you take it ("twice daily"), why you take it ("for blood pressure"), who prescribed it, and when you started. Mayo Clinic found that patients who bring accurate lists have 37% fewer medication errors. Many people forget supplements or over-the-counter pills, but those matter too. A daily aspirin or fish oil can interact with prescription drugs.
- Insurance card and ID: Even if you’ve been going to the same clinic for years, they need to verify your coverage. Some plans change networks yearly. If you’re not in-network, you could be billed unexpectedly.
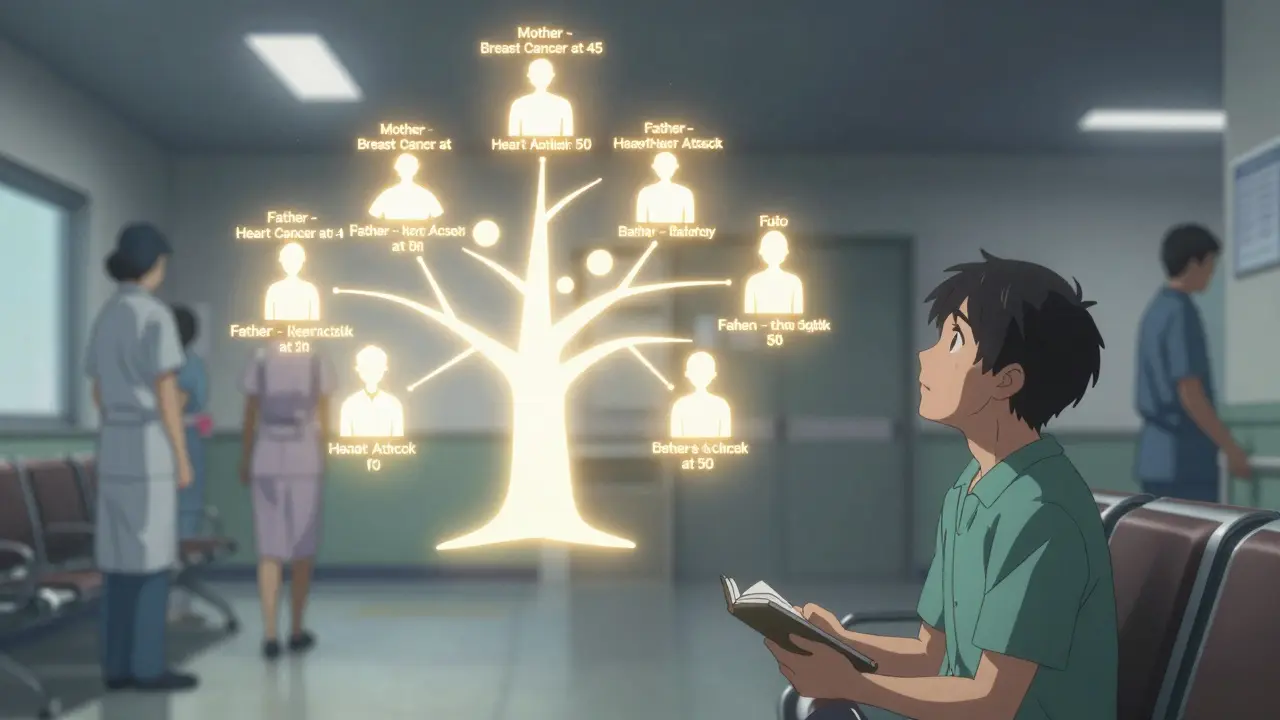
- Family health history: This isn’t just a formality. If your mother had breast cancer at 45, or your father had a heart attack at 50, that’s critical. Mayo Clinic specifically asks for three generations of health data on conditions like diabetes, cancer, and heart disease. This helps doctors spot patterns before symptoms even appear.
- Symptom log: Don’t rely on memory. Write down when symptoms started, how often they happen, how bad they are on a scale of 1 to 10, and what makes them better or worse. Did your headache only show up after coffee? Does your knee pain get worse after walking? Specifics like this help doctors rule out causes faster.
- Any recent test results: Blood work, X-rays, or EKGs from other clinics. If you had a test done elsewhere and didn’t get the results, call ahead. Don’t assume they’re in your file.
Some clinics now require digital check-ins. Cleveland Clinic’s AppointmentPass® system lets you scan a barcode at the front desk after submitting info online. If you’re going to a major health system, check their website before you leave home. You might save 20 minutes just by doing this.
What to Discuss: The 12 Critical Topics
Doctors have 15-20 minutes. If you don’t prioritize, you’ll leave with half your questions unanswered. Use this list to make sure nothing slips through.
- Medication changes: Are you taking something new? Stopped something? Had side effects? Even "I felt dizzy after starting this pill" matters. Many drug interactions go unnoticed because patients don’t mention supplements.
- New or worsening symptoms: Don’t say "I’ve been tired." Say "I’ve been exhausted by 3 p.m. for the last six weeks, even after sleeping 8 hours." Add details: weight loss, night sweats, changes in bowel habits, chest pressure, swelling in legs. These aren’t "just aging."
- Alcohol, smoking, and drug use: AdventHealth’s guidelines say doctors need exact numbers: "I drink 2 glasses of wine three nights a week," or "I smoked one pack a day for 15 years, quit in 2022." If you’re ashamed, remember: this isn’t about judgment. It’s about risk. Alcohol affects liver function. Smoking affects lung scans. Even occasional marijuana use can interfere with certain medications.
- Exercise habits: "I try to walk" isn’t enough. Say "I walk 20 minutes, five days a week." Or "I haven’t moved much since my hip surgery." Movement patterns tell doctors about heart health, joint stress, and mental well-being.
- As-needed medications: Did you use your inhaler last week? Take nitroglycerin for chest pain? Use ibuprofen for headaches? These aren’t "minor"-they’re warning signs. AdventHealth specifically requires these to be listed because they indicate uncontrolled conditions.
- Sleep quality: Do you snore? Wake up gasping? Fall asleep during the day? Sleep apnea isn’t just about tiredness-it raises stroke and heart attack risk.
- Mood and mental health: Are you feeling down, anxious, or overwhelmed? Doctors can’t treat what they don’t know. Even if you think it’s "just stress," it could be depression or burnout. The Institute for Healthcare Improvement found that patients who mention mood changes are 4x more likely to get timely support.
- Sexual health: Pain during sex? Changes in libido? New discharge? These are common but rarely brought up. Yet they can signal hormonal shifts, infections, or side effects from meds.
- Memory or focus issues: Forgetting names? Losing keys? Trouble following conversations? Don’t brush it off as "getting older." Early signs of cognitive decline can be slowed with intervention.
- Health goals: Do you want to lose weight? Lower your blood pressure? Get off a medication? Say it out loud. Doctors can’t help you reach goals you don’t name.
- Follow-up plans: Ask: "What happens next?" Should you repeat a test? See a specialist? Change your diet? Don’t leave without a clear next step.
- Questions about tests and treatments: Always ask: "Why are you recommending this?" "What are the side effects?" "What happens if I don’t do it?" And one powerful one: "What would you recommend if I were your mother/father?"

Why This Matters: The Real Impact
It’s not about being "perfect." It’s about giving your doctor the clearest possible view of your health.
St. Joseph Hospital Bangor tracked 1,200 patients over a year. Those who wrote down 3-5 questions before their visit had 89% of their main concerns resolved. Those who didn’t? Only 63%. That’s a 26-point gap-just from preparing.
Medication lists are the biggest gap. Mayo Clinic’s audit found that 45% of initial lists were wrong. People forget doses, mix up names, or leave out vitamins. One patient thought "Tylenol" was just for pain, not realizing it contained acetaminophen that was adding up with his liver meds. He nearly had liver failure.
And it’s not just about safety. It’s about time. Aurora Health Care measured appointment lengths and found that patients who submitted forms ahead of time saved 14.7 minutes per visit. That means more time to talk, more time to listen, more time to get it right.
Digital Tools That Help
You don’t have to write everything by hand anymore.
- MyChart (Cleveland Clinic): Lets you fill out symptom checkers before your visit. The system turns your answers into a structured report for your doctor.
- Mayo Clinic app: Can pull your pharmacy records directly from 27 major chains and sync with Apple Health or Google Fit. No manual entry needed.
- Ambetter Health: Automatically updates your medication list when you refill prescriptions through their mail-order pharmacy.
- AdventHealth’s LiveWell: Uses AI to suggest questions based on your past visits. If you’ve had high blood pressure three times in a year, it prompts you: "Did you monitor your BP this week?"
These tools aren’t gimmicks. They’re built on data from millions of appointments. And adoption is rising fast: 78% of major health systems now require pre-visit documentation.
What If You Forget Something?
You’re not alone. Most people walk in unprepared.
If you forgot your medication list, say: "I didn’t bring a list, but I can tell you what I’m taking right now." Then name each one clearly. If you didn’t track symptoms, say: "I’ve been having this issue for a few weeks, but I’m not sure how often." Your doctor will still help-you’ll just need more time.
Don’t cancel. Don’t feel embarrassed. Just show up. Preparation increases your odds. But even unprepared patients get care. The goal isn’t perfection. It’s progress.
Final Tip: Do This the Night Before
Set a 10-minute alarm the night before your appointment. Use it to:
- Grab your pill bottles and write down each one.
- Open your phone’s health app and check recent steps, heart rate, or sleep data.
- Write down the top 3 things you want to talk about.
- Put your ID, insurance card, and list in your wallet or bag.
That’s it. No fancy apps. No stress. Just three minutes of action that can change the outcome of your entire visit.
What if I don’t have a list of my medications?
Call your pharmacy. Most can email or print a list of all your current prescriptions. You can also log into your health insurer’s portal-many have medication records available online. If all else fails, bring your pill bottles. The labels have all the info doctors need.
Should I mention mental health concerns even if they seem minor?
Yes. Mental health is physical health. Feeling persistently down, anxious, or overwhelmed can affect your immune system, blood pressure, and sleep. Doctors can’t treat what they don’t know. Even if you think it’s "just stress," it might be depression, burnout, or a side effect of medication. There’s no judgment-just care.
Do I need to bring my family health history?
It’s not always required, but it’s one of the most powerful tools doctors have. If close relatives had heart disease, diabetes, or cancer before age 60, that increases your risk. You don’t need a full genealogy-just names, conditions, and ages at diagnosis. Mayo Clinic says this helps catch problems years before symptoms appear.
What if I’m nervous and forget what to say?
Bring a written list. Even a scrap of paper helps. You can also bring someone with you-a partner, friend, or adult child. They can help remember details, ask questions you didn’t think of, and support you if you feel overwhelmed. Most doctors welcome a second set of ears.
Can I text or email my doctor before the appointment?
Some clinics offer secure messaging through patient portals like MyChart. If yours does, send your list or questions ahead of time. It gives your doctor time to review and can shorten your visit. But don’t rely on texts or personal emails-they’re not secure or tracked in your medical record.
What if my doctor doesn’t ask about lifestyle factors like drinking or exercise?
Then bring it up. Doctors are busy, and they may assume you’ll mention it. But if you don’t, they won’t know. Say: "I’ve been thinking about my alcohol use and want to talk about it." Or: "I’ve been walking less lately-should I be concerned?" Taking the lead ensures you get the care you need.