When your kidneys aren't working well, what you eat matters more than ever. Protein is one of the most confusing parts of a kidney-friendly diet. Too much can overload your kidneys. Too little can leave you weak and malnourished. The right amount isn’t one-size-fits-all-it changes depending on how far your kidney disease has progressed. Understanding your protein targets for each stage of chronic kidney disease (CKD) can help you slow damage, avoid complications, and feel better every day.
What Protein Does (and Doesn’t Do) in Kidney Disease
Protein breaks down into waste products like urea and creatinine. Healthy kidneys filter these out. When kidneys are damaged, these wastes build up, causing fatigue, nausea, and itching. Cutting back on protein reduces this burden. But it’s not just about less protein-it’s about the right kind and the right amount.
Studies show that keeping protein intake in the right range can delay the need for dialysis by 6 to 12 months. That’s not just a number-it’s more time to live your life without needles or machines. But here’s the catch: if you cut protein too low, your body starts breaking down muscle. That leads to weakness, slower healing, and higher risk of infection. The goal isn’t starvation. It’s precision.
Protein Targets by CKD Stage
CKD is divided into five stages based on how well your kidneys filter blood. Your protein needs change at each step.
Stages 1 and 2 (GFR ≥60): Your kidneys are still working fairly well, but there’s early damage. Most guidelines recommend no more than 0.8 grams of protein per kilogram of ideal body weight per day. For someone who weighs 150 pounds (68 kg), that’s about 54 grams of protein daily. That’s roughly the amount in three eggs, a small chicken breast, and a cup of Greek yogurt. Some newer research suggests older adults in these stages may actually do better with slightly higher protein-up to 0.9-1.0 g/kg-to protect muscle mass. But if you have diabetes or high blood pressure, stick to the lower end.
Stages 3a and 3b (GFR 45-59 and 30-44): This is where most people start noticing symptoms-swelling, tiredness, trouble sleeping. Protein should drop to 0.55-0.60 g/kg/day. For a 150-pound person, that’s 40-50 grams daily. This is the critical zone where many people fall off track. Too little leads to wasting. Too much speeds up kidney decline. A 2024 study in JAMA Network Open found that older adults who ate more protein in this stage had lower death rates, likely because they were avoiding muscle loss. That’s why individualization matters.
Stages 4 and 5 (GFR 15-29 and under 15): Kidney function is severely reduced. Protein intake should be kept at 0.55-0.60 g/kg/day, but only if you’re not on dialysis. If you’re on dialysis, your needs jump up to 1.0-1.2 g/kg/day because dialysis removes protein. Many patients in stage 4 are advised to get half their protein from high-quality sources: eggs, milk, fish, chicken, lean beef, and soy. These contain all the essential amino acids your body can’t make on its own. Plant proteins like beans and lentils are easier on the kidneys but lack some of these amino acids. That’s why mixing them with animal proteins helps.
Animal vs. Plant Protein: What’s Better for Your Kidneys?
Not all protein is created equal. Animal proteins-meat, dairy, eggs-produce more waste per gram than plant proteins. They also release more phosphate and advanced glycation end products (AGEs), which cause inflammation and damage blood vessels. A 2021 meta-analysis found that replacing just 30% of animal protein with plant protein reduced the risk of kidney failure by 14% and lowered death risk by 11%.
But plant proteins come with trade-offs. Beans, lentils, and nuts are high in potassium and phosphorus-two minerals that build up in late-stage CKD. A cup of cooked lentils has 730 mg of potassium. That’s more than a banana. For someone in stage 4 or 5, that’s risky. Soy is an exception-it’s a complete plant protein with lower potassium than other legumes. Tofu and tempeh can be great options if portion-controlled.
Best strategy? Use a mix. Have one meal with animal protein (like grilled chicken) and another with plant protein (like a small portion of lentils with rice). This balances waste reduction with nutrient needs. Avoid processed meats like bacon or sausage-they’re high in salt, phosphate additives, and AGEs. Even small amounts can hurt.
Special Cases: Diabetes, Older Adults, and Muscle Loss
If you have both diabetes and CKD, protein targets get even trickier. Too little protein can make blood sugar harder to control. The American Diabetes Association recommends 0.8-0.9 g/kg/day for these patients. That’s slightly higher than standard CKD guidelines. The goal is to protect your kidneys without starving your muscles or spiking glucose.
Older adults face another problem: sarcopenia. That’s age-related muscle loss. Many people over 65 with CKD die from heart disease before ever reaching dialysis. Cutting protein too low can make them weaker and more likely to fall or get sick. Research shows higher protein intake (up to 1.0 g/kg) in this group improves survival-even if it means a slightly faster decline in kidney function. It’s a trade-off: quality of life vs. kidney longevity.
One in three people with stage 3-5 CKD develops protein-energy wasting. That means they’re losing muscle and fat even if they’re eating enough calories. This isn’t laziness-it’s a medical condition. Signs include clothes getting looser, weakness when climbing stairs, or not being able to get up from a chair without help. If you notice these, talk to your doctor. You may need special supplements like keto acid analogues (e.g., Ketosteril), which provide essential amino acids without the waste burden.
How to Actually Stick to Your Protein Target
Knowing the number is one thing. Hitting it every day is another. Most people struggle. A 2024 survey found that 74% of CKD patients felt constantly hungry on a low-protein diet. Another 62% said they felt weak. Social events became stressful. Family dinners turned into minefields.
Here’s what works:
- Use a protein tracker app: The National Kidney Foundation’s free Protein Target Calculator app lets you log meals and see your daily protein total in real time. Over 47,000 people have downloaded it since 2023.
- Meal prep with kidney-friendly recipes: Sites like Kidney Kitchen offer over 500 tested recipes with exact protein counts. Their content gets 1.2 million visits a month.
- Work with a renal dietitian: Patients who see a dietitian regularly are 3.2 times more likely to stick to their plan. Medicare now covers 3 hours of initial counseling and 2 hours of follow-up each year for CKD patients.
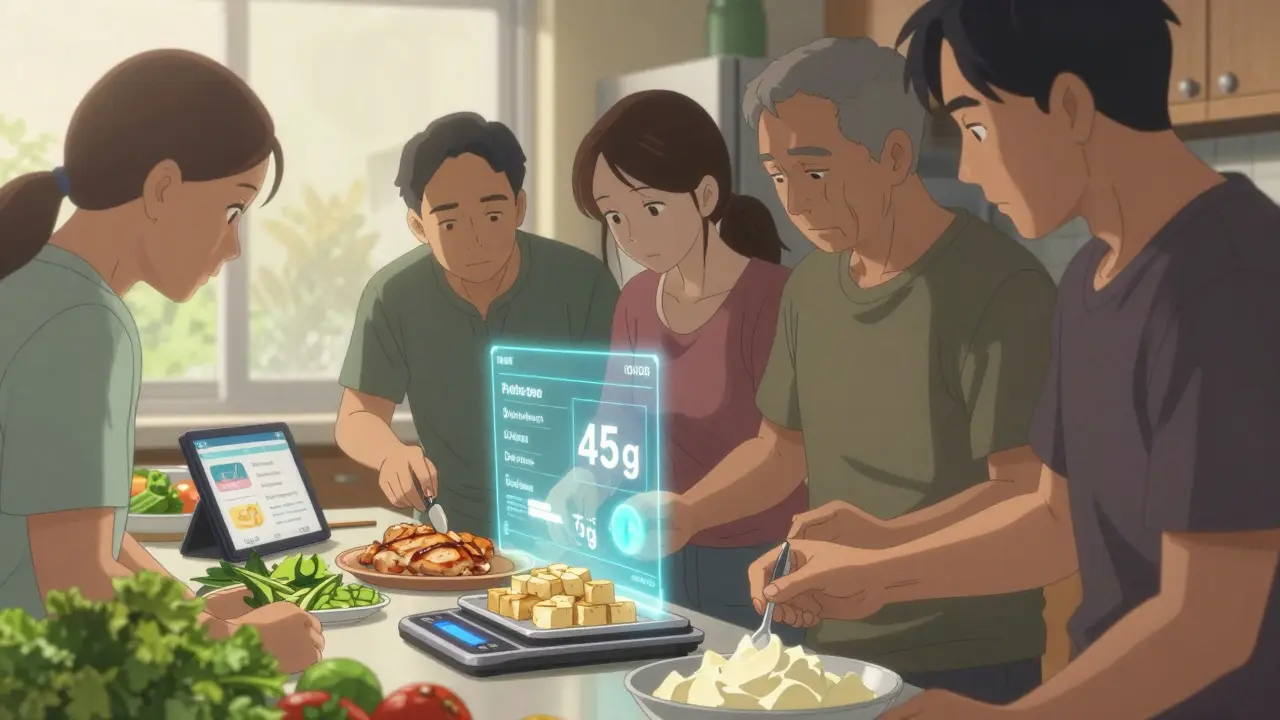
- Track mixed dishes: Soup, casseroles, stir-fries-these are protein traps. Use a food scale and check nutrition labels. Most people underestimate protein in these meals by 30-50%.
One patient on Reddit shared: “Cutting my protein from 100g to 45g made me feel like I was dying. Then I started working with a dietitian. We added egg whites, tofu, and low-protein bread. I didn’t feel hungry anymore. I started walking again.”
What’s New in Renal Nutrition
The field is moving beyond simple weight-based targets. New tools are emerging:
- Personalized protein algorithms use your age, blood urea levels, genetics, and even gut bacteria to predict your ideal intake.
- The NIH-funded PRECISE-CKD trial is testing whether measuring your daily urea production gives a better target than just your weight.
- Companies are developing plant-based protein powders with potassium removed-still in testing, but promising.
- Continuous glucose monitors are being studied to see how protein intake affects blood sugar spikes in diabetic CKD patients.
By 2030, experts agree: protein management won’t be about how much you eat-but what kind, when you eat it, and how your body responds.
Bottom Line: Find Your Balance
There’s no perfect number for everyone. Your protein target depends on your stage, age, muscle mass, diabetes status, and how you feel. The goal isn’t to eat as little as possible. It’s to eat just enough to protect your kidneys without wasting your body.
Start by asking your nephrologist for a referral to a renal dietitian. Get your ideal protein target in writing. Use an app to track your meals for a week. Adjust based on how you feel. And don’t be afraid to ask: “Is this helping me live better, or just delaying dialysis?” The best plan does both.
How much protein should I eat if I have stage 3 CKD?
For stage 3 CKD (GFR 30-59), aim for 0.55 to 0.60 grams of protein per kilogram of ideal body weight daily. For a 150-pound person, that’s about 40-50 grams per day. If you’re over 65 or have diabetes, your doctor may recommend slightly more-up to 0.8 g/kg-to protect muscle and energy levels. Always work with a renal dietitian to personalize this.
Can I eat plant-based protein with kidney disease?
Yes, but with caution. Plant proteins like tofu, tempeh, and seitan are easier on the kidneys because they produce less waste and phosphate. But beans, lentils, and nuts are high in potassium and phosphorus, which can be dangerous in stage 4 or 5. Stick to small portions and pair them with low-potassium foods. Soy is the best plant protein-it’s complete and lower in minerals. Always check your blood levels before increasing plant foods.
Why do I feel weak on a low-protein diet?
You may be losing muscle. Many people with CKD develop protein-energy wasting, especially if they cut protein too low. Feeling tired, weak, or unable to climb stairs are signs. Talk to your doctor. You may need to increase protein slightly, switch to high-quality sources like egg whites or whey isolate, or take keto acid supplements. Don’t ignore weakness-it’s not normal.
Do I need to count protein if I’m not on dialysis?
Yes. Even if you’re not on dialysis, protein intake directly affects how fast your kidneys decline. Studies show that eating too much protein accelerates kidney damage in stages 3-5. Counting helps you stay in the safe range-usually 0.55-0.8 g/kg/day. Use an app like the NKF’s Protein Target Calculator. It takes just 5 minutes a day and can save your kidneys.
Is there a difference between protein for CKD and dialysis patients?
Big difference. Before dialysis, you want to limit protein to 0.55-0.60 g/kg to reduce waste buildup. After dialysis starts, you need 1.0-1.2 g/kg because dialysis removes protein from your blood. Many patients are shocked when their protein needs jump after starting treatment. Your dietitian will adjust your plan immediately after dialysis begins.