Statin Interaction Risk Checker
This tool helps you understand your risk of myopathy (muscle damage) when taking statins based on your medications and personal health factors. The risk depends on which statin you're taking, what other medications you're on, and your individual health profile.
Most people taking statins never have serious muscle problems. But for some, even a small change in their medication routine can trigger muscle pain, weakness, or worse - a rare but dangerous condition called myopathy. The real danger isn’t the statin itself. It’s what it’s mixed with.
Why Some Statins Are Riskier Than Others
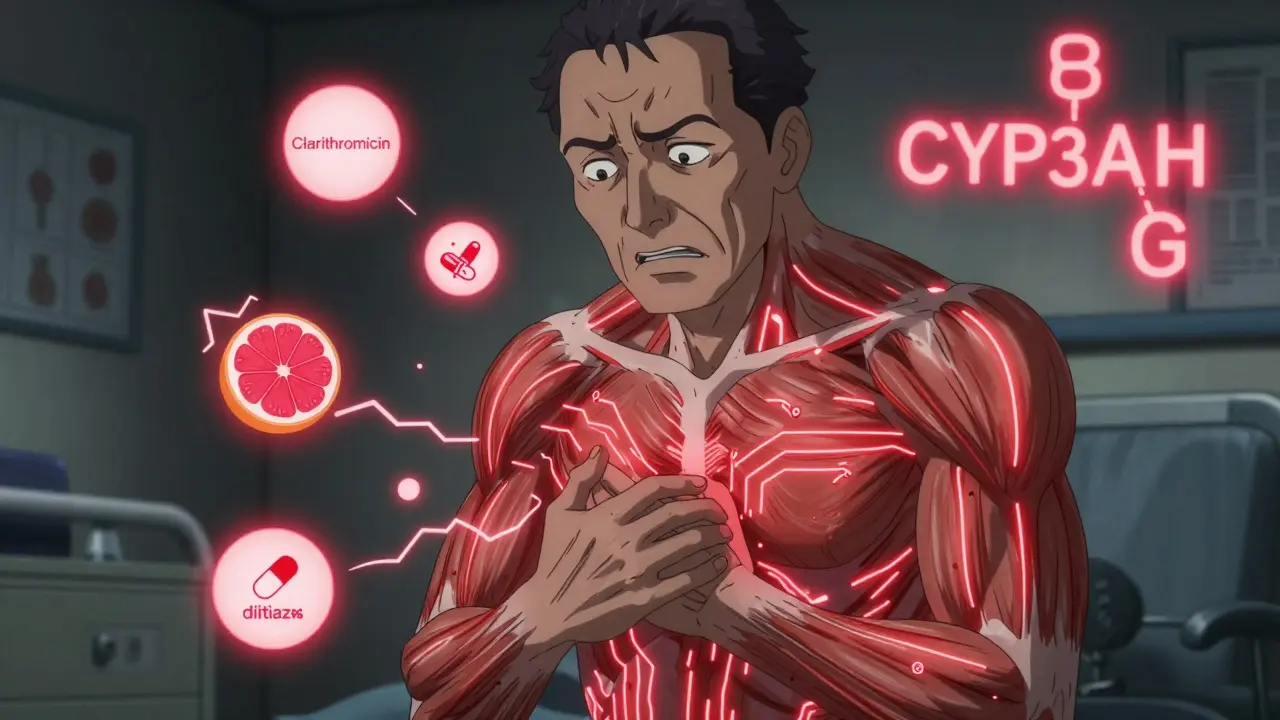
Not all statins are created equal when it comes to muscle risk. The difference comes down to how they’re processed in your body. Statins like simvastatin and lovastatin are broken down by an enzyme called CYP3A4. That’s the same enzyme that processes many common antibiotics, heart meds, and even grapefruit juice. When these drugs are taken together, your body can’t clear the statin fast enough. Levels build up. And that’s when muscle damage starts.Atorvastatin is also partly processed by CYP3A4, so it carries moderate risk. But pravastatin, rosuvastatin, and fluvastatin? They’re handled differently - mostly by the liver’s transporters, not CYP3A4. That makes them much safer to use with other meds.
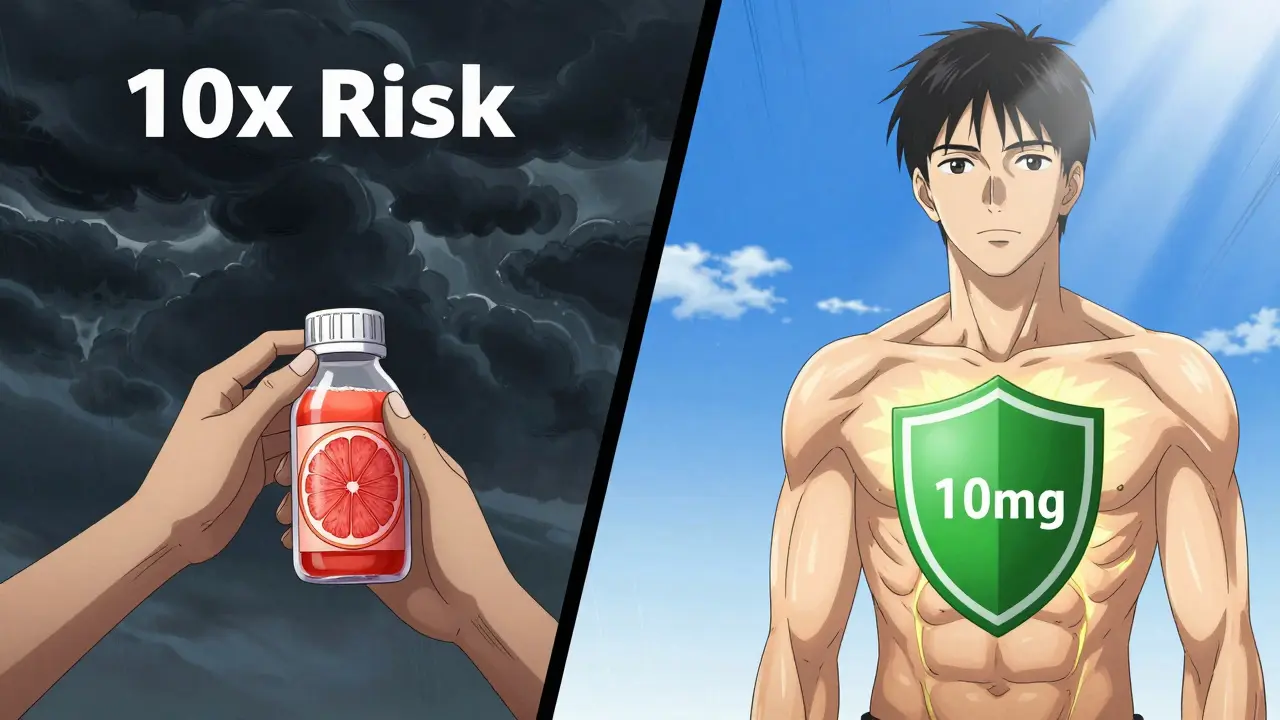
Here’s the reality: if you’re on simvastatin 80mg, your risk of myopathy is five to ten times higher than someone on the same dose of another statin. That’s why the European Atherosclerosis Society and the FDA both recommend avoiding simvastatin 80mg entirely. Even lower doses become risky when paired with the wrong drugs.
The Worst Culprits: Medications That Boost Statin Levels
Some drugs are red flags when taken with statins. The biggest offenders:- Clarithromycin and erythromycin - These macrolide antibiotics can spike simvastatin levels by up to 10 times. Azithromycin? Safe. It doesn’t interfere with CYP3A4.
- Cyclosporine - Used after organ transplants, this drug can increase statin levels by 3 to 13 times. That’s a massive jump. Even low-dose statins become dangerous.
- Gemfibrozil - A fibrate for triglycerides, it doubles statin levels and raises myopathy risk more than other fibrates like fenofibrate.
- Diltiazem and verapamil - These calcium channel blockers for high blood pressure are common. But with simvastatin, they’re a recipe for trouble. The FDA now limits simvastatin to 20mg max when taken with these drugs.
- Amiodarone - A heart rhythm drug. It’s also a CYP3A4 inhibitor. Combining it with high-dose simvastatin increases myopathy risk significantly.
It’s not just about the drug - it’s about the dose. A 10mg dose of simvastatin might be fine with a low dose of diltiazem. But 40mg? That’s where the danger spikes.
Who’s Most at Risk?
It’s not just drug interactions. Your body matters too. Certain people are far more likely to develop muscle problems:- Age 75+ - Older adults clear drugs slower. Their muscles are more sensitive.
- Small frame or low BMI - Less body mass means higher concentration of the drug in muscle tissue.
- Chronic kidney disease - Impaired kidneys can’t help flush out statin metabolites.
- Hypothyroidism - Low thyroid function slows metabolism, increasing statin exposure.
- Heavy alcohol use - Damages the liver, which is already working hard to process statins.
- Intense exercise - Strenuous activity stresses muscles. Add a statin that’s building up in your system? That’s a one-two punch.
One study found that 30% of people on statins report muscle pain or weakness. But in clinical trials, that number is often under 5%. Why the gap? Real life isn’t a controlled study. People take multiple meds. They’re older. They’re more active. They have other health issues. That’s where the real risk lives.
What to Do If You Feel Muscle Pain
Don’t ignore it. Muscle pain from statins isn’t like a sore leg after a workout. It’s deeper. Constant. Often in the shoulders, thighs, or back. It doesn’t go away with rest. You might feel weak - like climbing stairs is harder, or you can’t lift your arms.If you notice this:
- Stop taking the statin - but only after talking to your doctor.
- Get a creatine kinase (CK) blood test. A level over 10 times the normal upper limit confirms myopathy. Between 5 and 10 times? Your doctor should monitor closely.
- Review every medication you’re taking - including supplements, OTC painkillers, and herbal products.
- Don’t restart the same statin until the cause is clear.
Many people assume they’re statin-intolerant. But studies show 71% of those who quit statins due to muscle pain can tolerate a different one - especially if they switch to pravastatin or rosuvastatin at a lower dose.
Safe Alternatives and How to Manage Risk
If you need to stay on a statin but are on a risky drug, here’s what works:- Switch to pravastatin or rosuvastatin - These are the safest choices when combining with other meds. Rosuvastatin max dose should be 20mg if you’re on a CYP3A4 inhibitor.
- Temporarily stop the statin - If you’re on clarithromycin for 7 days, pause your statin during that time. Restart it the day after the antibiotic ends. No need to taper.
- Use lower doses - A 10mg dose of atorvastatin is far safer than 40mg, especially with interacting drugs.
- Consider non-statin options - Bempedoic acid (Nexletol) lowers cholesterol without entering muscle cells. It’s expensive - about $4,000 a year - but it’s a lifeline for people who can’t tolerate statins.
Coenzyme Q10 supplements are often suggested for muscle pain. The evidence is weak, but if you’re taking them and feel better, there’s no harm - unless your doctor says otherwise.
What’s New in 2026?
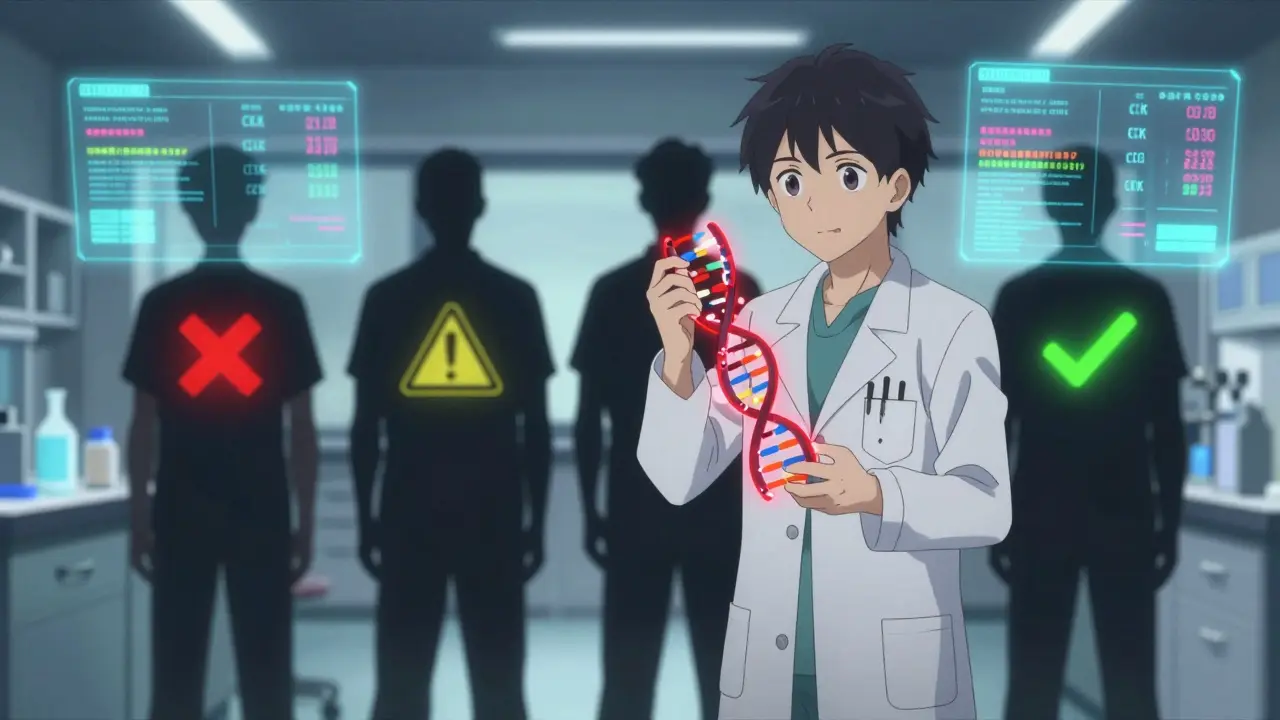
The field is moving fast. Genetic testing for the SLCO1B1 gene variant can now predict who’s at higher risk for simvastatin myopathy - up to 4.5 times higher. The FDA added this info to simvastatin labels back in 2011, but few doctors routinely test for it. That’s starting to change.Another promising idea: intermittent dosing. The 2023 DECLARE trial is testing whether taking rosuvastatin every other day reduces muscle side effects without losing heart protection. Early results look good.
And then there’s icosapent ethyl (Vascepa), approved for use with statins to cut heart attack risk. For some patients, this means they can use a lower statin dose and still stay protected.
Bottom Line: Don’t Panic, But Be Smart
Statins save lives. For people with high cholesterol, heart disease, or diabetes, the benefit far outweighs the risk. But that doesn’t mean you can ignore the red flags.Know your statin. Know your other meds. Tell your doctor everything - even the turmeric capsules or the OTC pain relievers. If you have muscle pain, don’t brush it off. Get a CK test. Switch if needed. You don’t have to suffer to stay healthy.
The goal isn’t to avoid statins. It’s to use them safely. And that means understanding what they interact with - and who’s most at risk.
Can I take ibuprofen with statins?
Yes, ibuprofen and other NSAIDs like naproxen don’t directly interfere with statin metabolism. But both can stress the kidneys, especially in older adults or those with existing kidney issues. If you’re taking statins long-term and also using NSAIDs daily, get your kidney function checked regularly. Occasional use for pain is generally fine.
Is grapefruit juice really dangerous with statins?
Yes - but only with certain statins. Grapefruit blocks CYP3A4 in the gut, which can raise levels of simvastatin, lovastatin, and atorvastatin. Even one glass can have an effect. Pravastatin, rosuvastatin, and fluvastatin are safe with grapefruit. If you love grapefruit, switch to one of those.
What if I forget to stop my statin before antibiotics?
If you took your statin while on clarithromycin or erythromycin for a day or two, don’t panic. Monitor for muscle pain, tenderness, or dark urine (a sign of muscle breakdown). Get a CK test if symptoms appear. In most cases, stopping the statin now and restarting after the antibiotic course is enough. Don’t restart until the antibiotic is fully finished.
Can I switch statins on my own if I have muscle pain?
No. Muscle pain can have many causes - including thyroid problems, vitamin D deficiency, or even overtraining. Stopping or switching statins without medical advice could leave you unprotected from heart disease. Always talk to your doctor first. They can check your CK levels, rule out other causes, and guide a safe switch.
Are generic statins safer than brand names?
Yes - and no. The active ingredient in generic statins is identical to brand names. But the inactive ingredients (fillers, coatings) can vary. For most people, this doesn’t matter. However, if you’ve had a reaction to one brand, switching to a different generic might help. Some people report fewer side effects with certain formulations. Talk to your pharmacist if you suspect this.
How often should I get my CK levels checked?
Routine CK checks aren’t needed for everyone. But if you’re on a high-risk statin (like simvastatin), taking interacting drugs, are over 75, or have kidney disease, get tested at baseline and then every 3-6 months. If you develop muscle symptoms, get tested immediately. Don’t wait.
Does taking statins at night reduce muscle risk?
No. The timing of statin doses doesn’t affect muscle risk. That myth comes from older statins like simvastatin, which are more effective at night because cholesterol production peaks then. But muscle side effects aren’t tied to timing. Take your statin when it’s easiest to remember - consistency matters more than the hour.
What Comes Next?
If you’ve been told you’re statin-intolerant, don’t give up. Many people just need the right statin, the right dose, or the right combination of meds. Talk to your doctor about switching to pravastatin or rosuvastatin. Ask about genetic testing if you’ve had repeated muscle issues. And if cost is a barrier, ask about patient assistance programs - many manufacturers offer them for bempedoic acid or other alternatives.Your heart health matters. But so does your quality of life. There’s a way to have both - if you know what to look for and who to ask.